Featured Articles
What separates high- and low-performing hospitals in 2025

Hospital finances showed signs of improvement at the end of the second quarter, though notable performance gaps remain between higher- and lower-performing facilities, according to Kaufman Hall’s latest “National Hospital Flash Report,” published Aug. 11.
The median monthly operating margin index rose to 3.7% in June, up from 1.9% in May, though the pace of improvement remains uneven and somewhat unexpected amid recent market turbulence.
Hospitals in the Northeast and Mid-Atlantic reported the largest year-over-year increases in operating margins at 38%, followed by the South and Midwest at 29%. The West and Great Plains saw declines of 13% and 27%, respectively. Smaller and mid-size hospitals generally fared better than large facilities: hospitals with 26 to 299 beds saw margin gains between 17% and 30%, while those with more than 500 beds experienced a 29% decline.
“Higher performing hospitals are nimbler on both the revenue and expense sides,” Erik Swanson, managing director and data and analytics group leader at Kaufman Hall, said in a news release. “They may be expanding their outpatient footprint, diversifying services or managing expenses like purchased services by centralizing some functions. They are also more likely to have value-based care or bundled care arrangements in place.”
In 2025, top-performing hospitals are setting themselves apart from lower-performing facilities through a combination of strategic, operational and financial factors. According to Kaufman Hall and Fitch Ratings, the key differentiators include:
1. Strong market presence in growth regions: Hospitals located in expanding markets — especially in the South, Midwest and Northeast — are benefiting from rising demand, better payer mixes and stronger revenue potential. These organizations are leveraging local demographics and economic growth to drive performance.
2. Workforce recruitment and retention. Talent remains a key differentiator. High performers are more successful in hiring and retaining clinical and nonclinical staff amid national shortages, allowing them to maintain service capacity and quality care while controlling labor costs.
3. Aggressive payer strategy: Top-tier hospitals are skilled at negotiating favorable payer contracts, often using a “mind the gap” approach to keep reimbursement rates at the upper end of the scale. These hospitals maximize market leverage to drive revenue growth.
4. Operational agility: High-performing hospitals are nimble and can adjust quickly to changing conditions. They centralize purchased services, optimize supply chains and adapt care models to improve efficiency.
5. Investment in technology and infrastructure: Successful systems are proactively investing in AI, health IT and data analytics. These investments support care delivery and administrative efficiency and prepare hospitals for value-based care and alternative payment models.
6. Outpatient expansion and service diversification: Expanding outpatient footprints and diversifying service lines allow top hospitals to meet evolving patient demand and offset pressures on inpatient care, particularly in high-cost settings.
7. Proactive real estate and capital management. Strong performers are strategically managing real estate assets to bolster balance sheets and fund growth initiatives, such as facility modernization and digital transformation.
In contrast, lower-performing hospitals, often in rural or underserved regions, struggle with:
- Limited access to capital
- Declining patient volumes or poor payer mixes
- Severe staffing shortages
- High dependency on public reimbursement
- Little room for investment in innovation or infrastructure
Fitch warns that this divergence is becoming a “trifurcation” of hospital performance, with institutions separating into top-tier, middle-tier and lower-tier segments. Without strategic shifts, the financial gap may widen in the years ahead.
Top-performing hospitals will “have a predisposition to maximize that market essentially with annual payer negotiations, in a ‘mind the gap’ mentality that keeps them at the upper end of the payment scale,” Fitch said in a recent report.
Meanwhile, most hospitals are expected to remain in a middle band: operating sustainably but with limited margin growth and persistent staffing challenges. Those at the bottom of the scale face declining volume and payer mix issues and will likely need to rely heavily on outside cash to stabilize, according to Fitch.
The latest hospital financial reports indicate that 2025 performance gains are unevenly distributed, with the gap between top and bottom performers potentially widening as financial pressures persist.

How to Get a High Paying Contract Nursing Job
Contract nursing offers the chance to do meaningful work, gain diverse experience, and earn competitive pay. Whether you’re pursuing contract nursing jobs, per diem nursing positions, or rapid response assignments, the key to maximizing your income is preparation and strategy.
If you’re ready to secure a high-paying contract nursing job, use these proven tips to set yourself apart and negotiate pay that reflects your expertise.
Your resume is your first impression. A clear, polished resume highlights your skills, certifications, and professional accomplishments, and it determines whether you’ll be invited to interview.
Include:
- Your nursing specialties (such as ICU, emergency department, or medical imaging)
- Certifications (like ACLS, BLS, or specialty credentials)
- Details about your experience in different care settings, such as inpatient care, skilled nursing facilities, or acute care staffing
It’s normal to have employment gaps but be ready to confidently explain them during interviews. A well-organized resume positions you as a serious professional ready for high-paying nursing contracts.
Keeping your credentials updated makes you a more attractive candidate and can improve your earning potential.
Make sure to:
- Renew essential licenses and certifications promptly.
- Consider adding specialty certifications that are in demand for travel nursing jobs and contract assignments.
- Stay up to date with immunizations required by hospitals and clinics. Being ready with all documentation can speed up onboarding and help you access crisis response nursing jobs or urgent needs contracts that often pay premium rates.
The more prepared you are, the easier it is for a nurse staffing agency or recruiter to match you with higher-paying positions.
Professional references can be the deciding factor in landing a top-paying assignment.
Employers and recruiters rely on references to verify your:
- Clinical skills
- Professionalism
- Reliability
Choose references who can confidently speak to your work ethic and performance. Positive recommendations can open the door to flexible nursing shifts, per diem contracts, and specialized roles that pay more.
Flexibility is often rewarded in the world of contract nursing.
Consider these options to boost your pay:
- Accepting night shifts or weekends, which usually come with higher hourly rates.
- Taking assignments in locations experiencing shortages, such as rural facilities or emergency department nursing jobs.
- Being open to rapid response contracts or crisis response assignments, which often offer premium compensation.
When you demonstrate a willingness to adapt, you make yourself more valuable to medical staffing agencies and healthcare employers.
In contract nursing, your reputation follows you from one facility to the next. A strong track record makes it easier to secure higher-paying contracts and preferred assignments.
Tips for maintaining a great reputation:
- Be punctual and dependable.
- Communicate clearly with staffing agencies and supervisors.
- Go the extra mile to provide excellent patient care.
Facilities are willing to pay more to bring on nurses with proven reputations for excellence.
Being a contract nurse offers countless benefits, from career variety to premium pay. To make the most of your opportunities:
- Invest time in preparing a strong resume.
- Keep certifications and immunizations current.
- Maintain excellent references.
- Stay flexible with shifts and assignments.
- Build and protect your professional reputation.
When you combine preparation with dedication, you can consistently secure high-paying contract nursing jobs that match your skills and goals.
If you’re looking for your next opportunity, Staff Relief, Inc. is here to help. We partner with hospitals, clinics, and healthcare facilities to connect nurses with the best assignments in Georgia and beyond.
Contact us today to explore available contracts and start earning what you deserve.

Hiring More Nurses Generates Revenue for Hospitals
Underfunding is driving an acute shortage of trained nurses in hospitals and care facilities in the United States. It is the worst such shortage in more than four decades. One estimate from the American Hospital Association puts the deficit north of one million. Meanwhile, a recent survey by recruitment specialist AMN Healthcare suggests that 900,000 more nurses will drop out of the workforce by 2027.
American nurses are quitting in droves, thanks to low pay and burnout as understaffing increases individual workload. This is bad news for patient outcomes. Nurses are estimated to have eight times more routine contact with patients than physicians. They shoulder the bulk of all responsibility in terms of diagnostic data collection, treatment plans, and clinical reporting. As a result, understaffing is linked to a slew of serious problems, among them increased wait times for patients in care, post-operative infections, readmission rates, and patient mortality—all of which are on the rise across the U.S.
Tackling this crisis is challenging because of how nursing services are reimbursed. Most hospitals operate a payment system where services are paid for separately. Physician services are billed as separate line items, making them a revenue generator for the hospitals that employ them. But under Medicare, nursing services are charged as part of a fixed room and board fee, meaning that hospitals charge the same fee regardless of how many nurses are employed in the patient’s care. In this model, nurses end up on the other side of hospitals’ balance sheets: a labor expense rather than a source of income.
For beleaguered administrators looking to sustain quality of care while minimizing costs (and maximizing profits), hiring and retaining nursing staff has arguably become something of a zero-sum game in the U.S.
But might the balance sheet in fact be skewed in some way? Could there be potential financial losses attached to nurse understaffing that administrators should factor into their hiring and remuneration decisions?
Research by Goizueta Professors Diwas KC and Donald Lee, as well as recent Goizueta PhD graduates Hao Ding 24PhD (Auburn University) and Sokol Tushe 23PhD (Muma College of Business), would suggest there are. Their new peer-reviewed publication* finds that increasing a single nurse’s workload by just one patient creates a 17% service slowdown for all other patients under that nurse’s care. Looking at the data another way, having one additional nurse on duty during the busiest shift (typically between 7am and 7pm) speeds up emergency department work and frees up capacity to treat more patients such that hospitals could be looking at a major increase in revenue. The researchers calculate that this productivity gain could equate to a net increase of $470,000 per 10,000 patient visits—and savings to the tune of $160,000 in lost earnings for the same number of patients as wait times are reduced.
“A lot of the debate around nursing in the U.S. has focused on the loss of quality in care, which is hugely important,” says Diwas KC.
But looking at the crisis through a productivity lens means we’re also able to understand the very real economic value that nurses bring too: the revenue increases that come with capacity gains.Diwas KC, Goizueta Foundation Term Professor of Information Systems & Operations Management
“Our findings challenge the predominant thinking around nursing as a cost,” adds Lee. “What we see is that investing in nursing staff more than pays for itself in downstream financial benefits for hospitals. It is effectively a win-win-win for patients, nurses, and healthcare providers.”
To get to these findings, the researchers analyzed a high-resolution dataset on patient flow through a large U.S. teaching hospital. They looked at the real-time workloads of physicians and nurses working in the emergency department between April 2018 and March 2019, factoring in variables such as patient demographics and severity of complaint or illness. Tracking patients from admission to triage and on to treatment, the researchers were able to tease out the impact that the number of nurses and physicians on duty had on patient throughput. Using a novel machine learning technique developed at Goizueta by Lee, they were able to identify the effect of increasing or reducing the workforce. The contrast between physicians and nursing staff is stark, says Tushe.
“When you have fewer nurses on duty, capacity and patient throughput drops by an order of magnitude—far, far more than when reducing the number of doctors. Our results show that for every additional patient the nurse is responsible for, service speed falls by 17%. That compares to just 1.4% if you add one patient to the workload of an attending physician. In other words, nurses’ impact on productivity in the emergency department is more than eight times greater.”
Adding an additional nurse to the workforce, on the other hand, increases capacity appreciably. And as more patients are treated faster, hospitals can expect a concomitant uptick in revenue, says KC.
“It’s well documented that cutting down wait time equates to more patients treated and more income. Previous research shows that reducing service time by 15 minutes per 30,000 patient visits translates to $1.4 million in extra revenue for a hospital.”
In our study, we calculate that staffing one additional nurse in the 7am to 7pm emergency department shift reduces wait time by 23 minutes, so hospitals could be looking at an increase of $2.33 million per year.Diwas KC
This far eclipses the costs associated with hiring one additional nurse, says Lee.
“According to 2022 U.S. Bureau of Labor Statistics, the average nursing salary in the U.S. is $83,000. Fringe benefits account for an additional 50% of the base salary. The total cost of adding one nurse during the 7am to 7pm shift is $310,000 (for 2.5 full-time employees). When you do the math, it is clear. The net hospital gain is $2 million for the hospital in our study. Or $470,000 per 10,000 patient visits.”
These findings should provide compelling food for thought both to healthcare administrators and U.S. policymakers. For too long, the latter have fixated on the upstream costs, without exploring the downstream benefits of nursing services, say the researchers. Their study, the first to quantify the economic value of nurses in the U.S., asks “better questions,” argues Tushe; exploiting newly available data and analytics to reveal incontrovertible financial benefits that attach to hiring—and compensating—more nurses in American hospitals.
We know that a lot of nurses are leaving the profession not just because of cuts and burnout, but also because of lower pay. We would say to administrators struggling to hire talented nurses to review current wage offers, because our analysis suggests that the economic surplus from hiring more nurses could be readily applied to retention pay rises also.Sokol Tushe 23PhD, Muma College of Business
For state-level decision makers, Lee has additional words of advice.
“In 2004, California mandated minimum nurse-to-patient ratios in hospitals. Since then, six more states have added some form of minimum ratio requirement. The evidence is that this has been beneficial to patient outcomes and nurse job satisfaction. Our research now adds an economic dimension to the list of benefits as well. Ipso facto, policymakers ought to consider wider adoption of minimum nurse-to-patient ratios.”
However, decision makers go about tackling the shortage of nurses in the U.S., they should go about it fast and soon, says KC.
“This is a healthcare crisis that is only set to become more acute in the near future. As our demographics shift and our population starts again out, demand for quality will increase. So too must the supply of care capacity. But what we are seeing is the nursing staffing situation in the U.S. moving in the opposite direction. All of this is manifesting in the emergency department. That’s where wait times are getting longer, mistakes are being made, and overworked nurses are quitting. It is creating a vicious cycle that needs to be broken.”
Goizueta faculty apply their expertise and knowledge to solving problems that society—and the world—face. Learn more about faculty research at Goizueta.
*Ding, Tushe, Kc, Lee: “Frontiers in Operations: Valuing nursing productivity in emergency departments.” Manufacturing & Service Operations Management 26:4:1323-1337 (2024)

Georgia could see the largest shortage of RNs by 2036
Staffing is one of the biggest issues facing ASCs. A 2023 survey from ORManager found that in the last 12 months, 56% of ASCs reported an increase in volume. Despite this success, 68% of facilities also reported having a more difficult time recruiting experienced operating room nurses.
“I think the biggest threat towards ASCs in 2023 is staffing, especially qualified, experienced staffing in all areas of an ASC, including business office, pre-op, OR (both nursing and surgical technicians), post-anesthesia care unit and recovery nurses. In addition, sterile processing technicians,” Michael Powers, administrator of Knoxville, Tenn.-based Children’s West Surgery Center, told Becker’s. “Each of these areas require a certain set of skills that are acquired and honed over time. There is increased competition, and in fact it is hard to compete with large health systems/hospitals. I am also finding that ASCs are competing in the same region against one another for the available staffing pool.”
The HRSA report highlights nurse workforce projections from 2021 to 2036 generated using the agency’s health workforce simulation.
Here are the five states with the largest projected shortages of registered nurses by 2036, per the report:
1. Georgia: 29% projected shortage
Projected vacancies: 34,800
2. California: 26% projected shortage
Projected vacancies: 106,310
3. Washington: 26% projected shortage
Projected vacancies: 22,700
4. New Jersey: 25% projected shortage
Projected vacancies: 24,450
5. North Carolina: 23% projected shortage
Projected vacancies: 31,350
https://www.beckersasc.com/leadership/5-states-facing-the-biggest-nurse-shortages-by-2036
Breaking News
How health system leaders combat ‘meeting overload’
Two-thirds of workplace leaders cite meetings as the No. 1 thing they spend too much time on, according to a Feb. 10 Korn Ferry article.
The figure stems from surveys of executives from Fortune and Korn Ferry’s 28th annual list of the World’s Most Admired Companies — on which six health systems, including Nashville, Tenn.-based HCA Healthcare and King of Prussia, Pa.-based Universal Health Services, earned a spot.
To counter meeting fatigue, Korn Ferry recommends organizations set clear expectations, including ground rules for length and participation. Meeting-free Fridays and daily windows for focused work time are also common across industries.
Hospital and health system leaders shared their strategies for managing meeting load with Becker’s. Intentional time management is key, according to Cliff Wilson, president and CEO of Albuquerque, N.M.-based Lovelace Health System.
“One thing I’ve learned as a leader is that if you’re not intentional with your time, your calendar will run your day,” Mr. Wilson told Becker’s. “In a virtual‑first environment, meetings can multiply quickly, so I focus my schedule on the goals that matter most and regularly evaluate what truly drives impact.”
Mr. Wilson treats one-on-one time with direct reports as nonnegotiable, as those conversations create alignment and support.
“I also protect time with frontline team members,” he said. “Being present in our facilities provides insights you can’t get from dashboards and helps build trust with the people caring for patients every day.”
He also periodically reviews his calendar to clear out low-value or outdated commitments.
“AI has been helpful in highlighting patterns and surfacing opportunities to reclaim time for strategic work,” he said. “Intentional time management isn’t just a habit, it’s a leadership discipline.”
Other health system leaders have eliminated redundant meetings to make better use of time. For example, Bob Duncan, executive vice president and COO of Hartford-based Connecticut Children’s, told Becker’s in June that the system replaced a one-hour report-out with a focused 30-minute huddle, prioritizing key themes and next steps. Carol Dozier, CEO of North King’s Daughters’ Health in Madison, Ind., also consolidated meetings to make better use of leaders’ time.
“Combining topics has enhanced the meeting content so we feel we have more meaningful discussions with different perspectives,” Ms. Dozier said.
The post How health system leaders combat ‘meeting overload’ appeared first on Becker’s Hospital Review | Healthcare News & Analysis.
The next phase of patient experience
Nearly half of hospital executives said patient experience is their top priority for the next two years, according to a recent survey. However, scores have steadily declined since 2019.
In 2020, 14% of executives said patient experience was their top strategic initiative. In 2025, that rose to 49%. However, patients’ “likelihood to recommend” scores have declined 2.2 points since 2019 — the only setting to see a decline. The corresponding scores have improved 2.8 points for medical practices, 1.7 points for ASCs and 0.5 points for emergency departments.
Becker’s asked nine leaders what levers hospitals can pull this year to have the greatest impact on patient experience. A single theme emerged: clear communication with patients.
Note: Responses have been lightly edited for length and clarity.
Jen Bayersdorfer. Chief Quality Officer at Providence St. Joseph Health (Renton, Wash.): The single greatest lever hospitals can pull is making coordination of care reliable and visible at the bedside. When patients clearly understand who is caring for them, what the plan is, what happens next and how transitions will occur, experience improves across multiple domains simultaneously, including nurse communication, discharge information, care transitions and overall rating. Standardizing practices such as bedside shift report, interdisciplinary rounding, purposeful hourly rounding and proactive discharge planning creates consistency in the patient journey rather than isolated service behaviors. This is all possible with a renewed focus on team-based, human-centered care.
Theresa Brennan, MD. Chief Medical Officer at University of Iowa Health Care (Iowa City): It is important to clarify the connection between patient experience, staff engagement and quality outcomes. This shifts the conversation toward measurable results rather than perception alone. We know that higher staff engagement and a strong culture of safe, high-quality care are directly associated with better patient satisfaction.
An exceptional patient experience happens when everyone involved in a patient’s care consistently communicates clearly and leads with empathy. Given the complexity of care, many people interact with patients during their encounters. Getting everyone on the healthcare team aligned with the patient’s needs and these expectations of every patient, every time, can be a challenge. There is increasing recognition of the impact patient experience has on overall quality outcomes, making it a priority for improvement efforts. Across the country, organizations are implementing operational changes such as structured bedside handoffs and nurse leader rounding to strengthen communication and enhance the patient experience.
Chris Cable, MD. Clinical Lead for Risant Health (District of Columbia): Across the healthcare industry, patients encounter significant variability in emergency department boarding times based on when they seek care — what day of the week or what week of the year they happen to need our help. This cannot be the case if we want our patients to have the best experience and outcomes in our hospitals.
Risant Health is focused on eliminating inconsistency in ED boarding and is already making progress with our Care Without Delay system. By adjusting how we do things behind the scenes, like staffing plans and rounding routines, we can make a big impact on how patients move into, through and out of our emergency departments. Not only is this a major driver of patient experience, we also know from evidence that quality outcomes are higher when patients spend less time waiting in the ED and more time in the hospital, where a full array of services are available. Since implementing Care Without Delay at Geisinger Community Medical Center a year ago, ED boarding hours have decreased by 55%, or more than 5,600 hours per month compared with the baseline.
Flavia Diaz-Hays, MSN, APRN. Vice President of Quality and Patient Safety at El Paso (Texas) Children’s Hospital: The biggest lever that hospitals can pull this year to improve patient experience is doubling down on the reliability and consistency of communication throughout the patient’s journey. In our opinion, patient experience boils down to how informed, respected and emotionally connected patients and families feel during their care journey. Of course clinical outcomes matter, but often patients and families determine if they received high-quality care by if the staff listened to them, explained things in a way that they could understand, and worked together like a team. If hospitals hardwire the discipline of standardized interdisciplinary bedside rounding, leader visibility and service recovery done in real time, we can create much more reliable and consistent experiences for our patients and families. When we focus less on “Is Sally a good communicator?” and more on “Did we communicate with Sally at the expected times throughout her stay?” we will see patient trust and experience increase.
There are a few things that have changed that allow us to leverage improvement in patient experience: 1) We, as executives and board members, understand that patient experience is not a variable to safety and quality — it is safety and quality. 2) We have real-time data available to us now to identify gaps in experience and intervene before they become system problems. 3) We are investing more than ever in our workforce to understand that employee engagement directly correlates to patient experience. 4) We are embracing high reliability principles, leadership rounding and accountability structures that force us to focus on the patient experience as part of our daily operations.
Alexander Greengold. Senior Vice President and Chief Consumer Experience Officer at Memorial Hermann Health System (Houston): When hospitals make the patient experience predictable, transparent and human, trust follows. At Memorial Hermann, we see the strongest impact from “ease of visit” behaviors like clear arrival guidance, proactive communication and consistent follow-through. By combining AI, real-time operational data and a deep understanding of the patient journey, we’re shifting from reacting to problems after they occur to predicting and preventing them.
Historically, the patient experience was treated as a survey score rather than an operational system. Feedback arrived weeks or months after the encounter — far too late to drive meaningful change — while accountability was fragmented, with no clear owner of the end-to-end journey. Experience improvement is more achievable now because data and technology have finally converged at the point of care. Hospitals can combine operational, digital and experience signals — not just lagging surveys — to predict dissatisfaction and intervene in real time, during the stay, rather than after the fact. At the same time, digital tools such as mobile check-in, real-time messaging, smart rooms and integrated rounding dashboards are embedded directly into care workflows, allowing teams to remove friction. At Memorial Hermann, this has enabled a shift from reactive service recovery to predictive, system-level experience design — allowing us to focus on the moments that matter most and scaling what works across our care delivery sites.
Lorie Rhine, MSN, RN. Chief Nursing Executive at UNC Health (Chapel Hill, N.C.): The most powerful lever is integrating patient experience with safety and quality, treating them as inseparable outcomes of reliable care. At UNC Health, our goal is to establish 100% trust with our patients, just as we strive for zero harm. When patients consistently feel safe, heard and cared for, their experience improves naturally.
At UNC Health, progress has accelerated through our proprietary care delivery model, Carolina Care, and the implementation of a standardized Nursing Bundle focused on safety and reliability. This bundle includes consistent interval nursing rounds, patient-engaged bedside report, and nurse and hospital leader rounding. Through these practices, nurses and leaders intentionally convey a clear message of safety and presence to patients. We support this work with standardized tools, leader education and clear accountability processes to ensure high fidelity across the system. Importantly, we measure not only process adherence through observation and validation, but also patient perception. We assess whether patients experience these safety-focused practices through nursing bundle questions on the HCAHPS survey and have recently added a systemwide patient-reported safety question to better understand whether patients feel safe while in our care.
Kristie Rozands, BSN, RN. Senior Director of Operations at Manning Family Children’s (New Orleans): The biggest lever for patient experience is communication with patients and families. Hospitals must ensure that families understand how to navigate the hospital environment, including outpatient services, inpatient care, diagnostic testing, discharge planning and billing processes. Clear, proactive communication reduces anxiety, builds trust and improves overall satisfaction. When families feel informed and supported, their experience improves — even during complex or stressful situations.
Historically, patient experience improvement has relied heavily on survey feedback. Many families are overwhelmed after hospitalization and may choose not to complete surveys, resulting in low response rates. This limits actionable data and often delays identification of communication gaps. Hospitals now have better tools, data visibility and structured processes to proactively engage families rather than relying solely on post-discharge surveys. By standardizing communication expectations and reinforcing accountability across teams, meaningful improvement is more attainable than ever.
Maureen Sullivan, BSN, RN. Vice President of Patient Experience and Service Excellence at MetroHealth (Cleveland): We lost some ground in consistently demonstrating our best practices [for patient experience] during the pandemic, and it takes time, focus and sustained effort to rebuild them. At MetroHealth, we’ve seen patients respond positively to our human‑centered training, particularly the emphasis on empathy. For example, historically the emergency department has been one of the most challenging care settings to consistently exceed patient expectations, and we’ve seen a steady improvement that has been sustained for the past year. What has made the greatest impact, however, is the commitment of clinical leadership to fostering a culture of excellence and accountability. This focus supports not only exceptional care for patients but also a positive, engaging and supportive environment for the staff who deliver that care.
Barbara Vazquez, DNP, RN. Chief Nursing Officer for Christus Children’s Hospital (San Antonio): The biggest opportunity we have right now is to give our caregivers more time to be fully present with patients and families. Competing demands such as documentation, technology, operational pressures often pull caregivers away from the bedside. Even the most dedicated team can struggle to deliver the kind of calm, consistent communication families deserve when the system makes it hard to do so. When nurses and care teams can slow down enough to listen, explain, and connect, everything about the experience improves. It’s not a new idea, but it’s the one that consistently makes the most meaningful difference.
The post The next phase of patient experience appeared first on Becker’s Hospital Review | Healthcare News & Analysis.
What’s next for hospital wages?
Hospitals are reaching a breaking point as demand and competition for healthcare workers pushes wages ever higher.
Labor and expenses per calendar day grew 5% from 2024 to 2025, and 12% from 2022, according to Kaufman Hall’s “National Hospital Flash Report” and the growth may not be done. Fitch forecasts staffing costs will rise in the mid-single-digit rates, while medical professional fees could increase by around 10%, a change from last year’s tailwinds as health systems reduced reliance on temporary staffing. The pressure stems from a fundamental tension: increased competition for a finite pool of qualified workers, compounded by a generational shift in workforce expectations, is forcing hospitals to rethink their compensation strategy from the ground up.
Nowhere is that rethinking more visible than in California, where legislation passed in 2024 raised the minimum wage for healthcare workers to $25, phased in over three years. The mandate doesn’t just affect entry-level roles; it elevates the pay scale for positions throughout the system, creating a cascade effect that strains already tight budgets.
For hospitals, especially rural and community organizations operating on thin margins, the pressure is spurring a search for new revenue-adding services and more creative ways to make ends meet.
“One of the most pressing workforce challenges we anticipate in 2026 is the continued increase in mandated minimum wages for healthcare workers in California,” said Marie Langley, CEO of Desert Valley Medical Group in Victorville, Calif. “While raising wages are necessary to keep pace with the region’s escalating cost of living and to provide meaningful opportunities for individuals entering the workforce, they also create significant wage compression for experienced staff who have invested years in developing their skills and expertise.”
Ms. Langley said the salary increases impact almost all entry-level positions and create a complex challenge for leadership to balance fairness, retention and morale for the more tenured employees. She also sees compensation expectations shifting and the pressure mounts as professional reimbursement rates stagnate or decline.
“To address this, we are proactively reviewing compensation structures, investing in career progression and professional development opportunities and identifying operational efficiencies to help offset rising labor expenses,” she said. “Our goal is to remain competitive, equitable and financially sustainable while continuing to support and invest in our workforce.”
California hospitals aren’t the only ones giving steep pay increases. In the last year, Becker’s recorded 44 hospitals and health systems that increased pay for some or all employees in clinical and non-clinical roles. In January, Charlotte, N.C.-based Advocate Health reported investing $776 million in workforce compensation this year, including a unified $18.85 minimum wage across all hospitals. Renton, Wash.-based Providence also committed $600 million in merit and market adjustments for staff this year as part of a strategic overview.
Jenny Collopy, vice president and chief marketing and communications officer of The Christ Hospital Health Network in Cincinnati, sees a growing disconnect between the cost of care delivery and what hospitals are paid for care.
“Wages for healthcare workers must continue to increase so team members can keep up with inflation, support their families and manage the rising cost of living,” she said. “At the same time, inflation continues to outpace what payers are willing to reimburse for healthcare services. That imbalance puts real pressure on health systems and forces difficult tradeoffs.”
The Christ Hospital is making adjustments through the Forward 2.0 operational improvement plan, focused on improving performance, eliminating inefficiencies and redesigning care so our teams can work at the top of their license. Then, the organization can reinvest in the workforce without negatively impacting access or quality of care.
The hospital’s Team Member Value Proposition focuses on ensuring team members have “everything it takes for everyone to thrive.”
“That means creating an environment where team members feel valued, have clear pathways for growth and mobility, are recognized and rewarded for excellence, and feel genuinely connected to our mission,” said Ms. Collopy. “Building a strong culture of engagement and loyalty is one of the most important drivers of retention, and it’s a commitment we take seriously as we navigate the workforce challenges ahead.”
Hiring healthcare workers is more competitive; health systems are investing in education pipelines, but that takes time and organizations are seeing an immediate need to increase compensation packages to maintain or expand access to care today. Physicians and nurses entering the workforce are seeking additional schedule flexibility, faster career growth tracks and more work-life balance.
Erika Werner, MD, president of the physician organization at Boston-based Tufts Medical Center, said historically hospitals expected 50-plus hour work weeks that could stretch all seven days of the week, and clinicians requested less time off for illness or family leave. In the academic setting, research and committee work were performed outside regular hours and considered “privileged pursuits.”
That’s not the case today.
“Not only are new hires challenging these historic healthcare norms, but seasoned clinicians are seeking culture change as they see their age-matched peers in other professions having increased schedule flexibility,” said Dr. Werner. “While this evolution has enormous potential to result in a happier, healthier workforce, reductions in clinician effort without congruent decreases in compensation risk further increases in labor costs, the main driver of ever escalating healthcare costs. Our health system is navigating these competing interests through honest, direct discussions between clinicians and administrators.”
The clinical and administrative leaders are developing a framework of understanding about how clinical and non-clinical time drives healthcare forward and delivers value. Together, the group is increasing transparency about the value of future investments.
“We are evolving our employment model so that clinicians can titrate time and compensation to best fit their individual needs,” said Dr. Werner. “Only with partnership, transparency and flexibility can we meet workforce and financial demands of 2026 and beyond.”
The post What’s next for hospital wages? appeared first on Becker’s Hospital Review | Healthcare News & Analysis.
EHR strategy becomes a recruitment lever for health systems
For many chief medical information officers, technology investments are no longer framed solely as operational upgrades. Increasingly, they are being discussed in the context of clinician recruitment, retention and burnout mitigation.
Becker’s asked CMIOs whether EHR platforms and newer AI tools are influencing their ability to attract and retain clinicians — and whether those technologies are making a measurable difference in workforce stability.
Several leaders pointed first to documentation burden and inbox overload as defining pressure points.
“Our EHR and newer AI tools are increasingly important to both recruiting and retention because they influence what matters most to clinicians in their daily work: time spent on documentation, inbox overload and how easily teams can work together,” said Usman Akhtar, MD, CMIO of VHC Health in Arlington, Va.
That emphasis on documentation time has fueled rapid expansion of ambient AI tools across health systems. At Norfolk, Va.-based Sentara Health, for example, leaders piloted a large language model to generate discharge summaries using episode-of-care data — a project that required retraining to eliminate early hallucinations before scaling systemwide. After rollout across 12 acute facilities, adoption surpassed 75%, driven largely by physicians who said the tool gave them meaningful time back.
For Joseph Evans, MD, vice president and chief health information officer at Sentara, those types of deployments now shape recruitment conversations.
“Our technology strategy has shifted from a purely operational focus to a primary lever for retention, where candidates now view relentless devotion to human-centered design and EHR usability as a proxy for how we value clinician time,” he said.
He added that ambient intelligence has rapidly evolved from novelty to “table stakes” as clinicians seek to minimize after-hours charting and administrative friction.
Other CMIOs said clinicians are watching not just for AI adoption, but for sustained signals that leadership understands burnout at a structural level.
“When physicians see a credible commitment to reducing inbox burden, streamlining workflows and reinvesting reclaimed time into patient care, it signals that leadership understands burnout and is willing to act on it,” said Amer Saati, MD, CMIO at Roseville, Calif.-based Adventist Health.
In some cases, that signal begins with infrastructure decisions rather than advanced AI. Adventist Health committed to a systemwide Epic transition in 2024 after a multiyear evaluation, underscoring how EHR environment and workflow cohesion are increasingly treated as strategic levers.
At Valley Health System in Paramus, N.J., clinician frustration with fragmented data and manual reconciliation prompted a move toward a unified platform.
“This decision was based on overwhelming feedback from our clinicians, who have been struggling with multiple sources of clinical data and having to manually reconcile data from within our own network each time they open a patient’s chart,” said CMIO K. Nadeem Ahmed, MD.
“It is unclear how this may help retain or attract clinicians; however, we are confident it will improve the overall experience for all our healthcare professionals in providing high-quality care to our patients,” he said.
Valley Health System’s broader digital strategy has also tied technology investments to measurable clinical outcomes. Its new hospital’s smart rooms integrate EHR data with AI-powered fall prevention alerts, reducing falls by 10% to 30% during pilot phases — an operational improvement leaders say reduces staff disruption and workflow strain.
CMIOs described a consistent pattern: Clinicians are evaluating employers not on whether they “have AI,” but on whether digital tools tangibly reduce cognitive load. Adoption rates, workflow integration and measurable time savings matter more than feature launches.
In that environment, technology investments are becoming less about innovation branding and more about daily usability — visible evidence that leadership is attempting to restore time to patient care.
The post EHR strategy becomes a recruitment lever for health systems appeared first on Becker’s Hospital Review | Healthcare News & Analysis.
Child obesity rates hit record high: 5 notes
One in 5 children aged 2 to 19 in the U.S. are living with obesity, marking the highest rate ever recorded, according to newly published data from the CDC.
The agency published two reports Feb. 25 examining obesity prevalence in the U.S. — one focused on children and adolescents and another on adults 20 and older. The estimates are based on measured height and weight data collected through the National Health and Nutrition Examination Survey between August 2021 and August 2023.
Five things to know:
1. About 21.1% of children and teenagers ages 2 to 19 are living with obesity, including 7% with severe obesity, according to the new data. By comparison, during the 1971-1974 survey cycle, 5.2% of children had obesity and 1% had severe obesity, underscoring the sharp rise over the past five decades.
2. Nearly 23% of adolescents ages 12 to 19 were classified as having obesity in the most recent survey, the highest prevalence among pediatric age groups. Among children ages 2 to 5, 14.9% were classified as obese.
3. About 40.3% of adults ages 20 and older met criteria for obesity in the 2021-2023 survey period. Of those, 9.7% had severe obesity, while 31.7% of adults were classified as overweight. The latest figure represents a substantial increase from 1988-1994, when 22.9% of adults had obesity, 2.8% had severe obesity and 33.1% were overweight.
4. In 2017-2018, 42.4% of adults were classified as having obesity — the highest level ever recorded in the survey. The decline to 40.3% in the most recent cycle suggests the rapid rise seen in earlier decades may be slowing, though experts told ABC News it is too early to determine whether the shift represents a sustained downward trend.
5. Public health experts say a combination of factors could be contributing to the leveling off among adults, including increased awareness of nutrition and physical activity, policy interventions and the growing use of GLP-1 drugs.
The post Child obesity rates hit record high: 5 notes appeared first on Becker’s Hospital Review | Healthcare News & Analysis.
Limiting loans for nurses will make our country’s health care crisis even worse
Proposed changes to federal student loans threaten to shrink the nursing workforce when we can least afford it.
Our nation is in the throes of a health care crisis, and we should be doing everything possible to support nurses and attract new ones to the profession. Yet, the Department of Education has officially proposed new rules that will limit access to federal loans for graduate education and exclude nursing from a list of “professional degree” programs eligible for higher financial support. This proposal risks making our crisis even worse.
By 2028, the U.S. is expected to be short more than 100,000 health care workers needed to provide essential care. Simultaneously, health care demand is accelerating due to an aging population and the growing prevalence of chronic diseases. This growing gap between workforce supply and patient need is already straining Americans’ access to timely, quality care.
If adopted, this change would sharply limit federal loan amounts and loan forgiveness pathways for post-baccalaureate nurses including our Advanced Practice Registered Nurses (APRNs), our nurse faculty, nurse leaders, researchers, scientists and other frontline providers. It’s a misguided move that would hurt not only current and future nurses, but patients and families across the country – at the exact moment our country can least afford it.
The Department of Education’s definition of “professional degree” for these loan caps includes disciplines we’d all expect and support: medicine, pharmacy, dentistry, optometry, and law, to name a few. Yet somehow, their approach overlooks nursing – even though nurses are, in many instances, the sole providers of essential health care services for patients and communities.
If federal policymakers leave nursing off the list of “professional degree,” nurses pursuing master’s or doctoral degrees would have access to roughly half as much federal student loan aid as other recognized professional degrees. Post-baccalaureate nursing students’ aggregate borrowing will be capped at $100,000, compared to $200,000 for degrees deemed professional. The annual borrowing limit would be just $20,500 for nursing, compared to $50,000 for recognized professional degrees. According to the National Center for Education Statistics, graduate nursing programs cost an average of more than $33,000 per year, already exceeding the proposed federal cap. Recent studies also show the average cost to be closer to $38,542. Many nurses interested in pursuing advanced roles and leadership positions will either be priced out of this educational pathway or will have to take out private loans which have higher interest rates. It also creates barriers, not only for nurses from rural, underserved or low-income backgrounds, but for the patients that rely on high-quality nursing care in communities across the country.
Each year, thousands of nurses depend on federal student loans to pursue advanced degrees to become nurse practitioners, certified registered nurse anesthetists, certified nurse midwives and clinical nurse specialists. These professionals are essential to broadening access to primary care, supporting rural hospitals and ensuring the stability of the health care workforce.
The ripple effects extend even further. In 2024 alone, U.S. nursing schools had 1,693 full-time faculty vacancies. Imposing these graduate loan caps would only deepen this faculty shortage by discouraging nurses from earning the degrees required to teach our next generation of nurses. We desperately need more new nurses entering the field. Without them the consequences will be evident across every setting where patients seek health care.
In a recent letter to the Department of Education, a bipartisan, bicameral group of more than 140 lawmakers urged the inclusion of nursing on the list of professional degrees eligible for full federal loan benefits, emphasizing the field’s critical contribution to the health care system. And more than 245,000 nurses and patients across the country have signed our petition calling on the Department of Education to reverse course.This is not just a trivial policy change. It will have enormous consequences, not only for the nursing profession but for all of us who will need nurses’ care. The Department of Education public comment period is now open. We urge all Americans, who have relied on the care of our nation’s nurses, to submit comments to regulations.gov urging the Department of Education to include post-baccalaureate nursing degrees (MSN, DNP, Ph.D.) explicitly in the list of “professional degrees.” Our nation’s health depends on it.
The post Limiting loans for nurses will make our country’s health care crisis even worse appeared first on Becker’s Hospital Review | Healthcare News & Analysis.
Radiologist turnover doubled in recent years, study finds
Job-switching rates among U.S. radiologists increased by 61% between 2013 and 2022.
After adjusting for radiologist and practice characteristics, researchers found odds of practice turnover, or the phenomenon of leaving one organization to join another, were about twice as high in 2020-2022 compared to 2013, according to a Feb. 24 study from the Harvey L. Neiman Health Policy Institute. The analysis examined 39,439 radiologists across 280,692 practice years.
Turnover rates were 6% higher among women than men, 12% higher in metropolitan areas, and 9% lower among academic radiologists than their nonacademic counterparts. Researchers also found a relationship between workload and turnover, with rates declining with increased work relative value units (wRVUs) up to a threshold before rising again.
That tipping point was 12,940 wRVUs overall, 8,820 for academic radiologists and 13,380 for nonacademic radiologists.
Researchers said the findings offer insight for health systems facing workforce shortages and rising burnout and attest to the importance of balancing workload with retention efforts.
The post Radiologist turnover doubled in recent years, study finds appeared first on Becker’s Hospital Review | Healthcare News & Analysis.
The workforce investments health system execs refuse to cut
As hospitals nationwide contend with margin pressure and persistent workforce shortages, 56 health systems were named to Forbes‘ annual list of America’s Best Large Employers.
Leaders from several of those organizations told Becker’s they have deliberately protected — and in some cases expanded — investments in leadership development, career pathways, employee well-being and benefits, even as labor costs rise.
Nationwide, labor expresses are increasing across nearly every region and hospital size, rising 5% year over year, according to a Nov. 12 Kaufman Hall report.
Rather than scaling back workforce spending, the executives described doubling down on internal talent pipelines, burnout prevention, employee recognition and programs designed to strengthen retention and engagement.
Below, leaders from 13 of the organizations featured on Forbes‘ list described the workforce investment they refused to cut in a year defined by financial headwinds.
Editor’s note: Responses have been lightly edited for clarity and length.
Alan Kaplan, MD. CEO of UW Health (Madison, Wis.): Our UW Health team provides remarkable care. With demand for our care always growing against a backdrop of national staffing shortages, we realize that following conventional wisdom in workforce development just isn’t enough. We’ve created an innovative set of “earn as you learn” apprenticeship programs we call our career pathways program. Through partnerships with local colleges, community groups and state government, we’ve created apprenticeship programs across key roles like registered nurse, respiratory therapist, medical assistant, nursing assistant, pharmacy technician and ophthalmology technician. Most of these programs were either first of their kind in the nation or first of their kind in Wisconsin, and they enable existing staff to further their careers while still working and at no cost to themselves. They also present an appealing entry point to careers in clinical care for new team members. Despite the national healthcare worker shortage, we’ve seen our retention rates benchmark at the 90th percentile in part due to these innovative programs. Despite the margin pressures faced across the healthcare sector, we’ve continued to invest in these programs, recently launching new apprenticeships for key surgical tech and MRI tech programs, further developing a model for success in a challenging labor market.
Beth Green. CHRO of Cooper University Health Care (Camden, N.J.): In healthcare, financial pressure is real — and that’s exactly why continuing to invest in leadership development matters. When times are hard, strong leadership isn’t a “nice to have,” it’s a necessity.
We know from experience that well‑prepared leaders drive engagement, retain talent, manage resources more responsibly, and keep teams focused on patients — even during uncertainty. Cutting back on leadership development may look like short‑term savings, but the long‑term costs — turnover, disengagement, slower decision‑making and burnout — are far greater.
That’s why we continue to invest in our leaders through formal leadership development programs, individual development plans, leadership assessments such as 360[-degree] feedback and other executive assessment tools and coaching. While we partner with external coaches for our executives, we’ve also built an internal leadership coaching program to support leaders at all other levels — ensuring access to development across the organization.
The return on investment is clear. Leaders who understand financial decision‑making, can adapt to new technology like AI, and know how to lead people through change make better choices every day. Those choices directly affect quality, safety, experience and financial performance.
At Cooper, investing in our leaders is one of the most effective ways to protect our future. When we support leaders, they support their teams — and that’s how we remain strong, resilient and focused on our mission, even in challenging times.
Calvin Allen. Executive Vice President and CHRO of Children’s Hospital of Philadelphia: We believe retention is our best recruitment strategy. When staff feel valued and supported, they become true ambassadors for our mission. During challenging financial times, it may be tempting to cut spending on programs that don’t show immediate returns. However, we see well-being and employee development as essential investments — integral to quality care, safety and our long-term financial health.
Instead of scaling back, we preserved and strengthened our well-being initiatives, with special attention to preventing burnout. Burnout and fatigue, especially among medical staff, lead to higher turnover and disengagement, which ultimately affect patient outcomes. Eliminating these supports might offer short-term relief, but would undermine our stability in the long run. We have clearly signaled to our workforce that their well-being is non-negotiable.
We also safeguarded programs that enrich the employee experience, such as tuition assistance, internal mobility and leadership development. Rather than relying on external hires, we invest in developing internal talent — creating clear career pathways for all employees. This approach boosts engagement, improves retention and reduces reliance on contract labor and expensive recruitment cycles.
By remaining committed to people-focused investments, we ensure a stable, engaged workforce dedicated to exceptional care and service.
Cliff Megerian, MD. CEO of University Hospitals (Cleveland): Despite ongoing margin pressures and rising labor costs, we made a deliberate decision not to cut investment in direct patient care. Protecting the teams who deliver care at the bedside remains our top priority, because maintaining quality, safety and patient experience is foundational to our mission.
Instead of reducing headcount, we formed revenue and expense cabinets that focused on identifying where we were not being reimbursed appropriately for the high‑quality care we provide. This work allowed us to capture revenue we had previously earned but not received. On the expense side, the teams concentrated on eliminating waste, inefficiencies, outdated processes and unnecessary spending that enabled us to keep our workforce intact.
We also accelerated the use of technology to streamline operations and bring work back in‑house, reducing or eliminating reliance on third‑party vendors. These strategies helped us protect critical clinical roles while still strengthening financial performance.
Duane McFadden. CHRO of Children’s Hospital Colorado (Aurora): Children’s Hospital Colorado recognizes the significant pressures created by rising labor costs, talent shortages in key specialty areas and the growing expectations placed on leaders in a highly volatile labor market. Despite these challenges, we believe this is not the time to divest in how we support our workforce. Instead, we have intentionally increased our investment in areas we believe strengthen engagement, retention and long‑term sustainability.
Growing our own talent pipeline: We have expanded programs that reach high schools, colleges and universities, and trade schools to build strong partnerships and create early pathways into our organization. Once team members join us, we support them in defining clear career paths and provide training, education and financial assistance to help them grow within our system.
Leadership development: We believe leadership capability is a critical differentiator in the team member experience. We have increased leadership development opportunities to ensure leaders are equipped not only to manage teams, but to lead in ways that are inspiring, values‑driven and deeply connected to our mission.
Benefits and well‑being: We’ve expanded our benefits portfolio while, in many cases, reducing premiums and out‑of‑pocket costs for team members. These investments are already delivering meaningful improvements in satisfaction and engagement.
Jim VanderSteeg. President and CEO of Covenant Health (Knoxville, Tenn.): When hospitals face financial pressure, it’s tempting to pull back on workforce development. We did the opposite.
Over the past 12 months, we protected our investments in employee growth and career development. We didn’t touch them — because cutting now would cost us the next generation of caregivers.
As a not-for-profit healthcare system, our measurement of success is the pursuit of our mission. Every dollar we save goes back into care. We believe the quality of care depends entirely on the quality of the people delivering it. Every dollar we spend developing our team is a dollar that keeps an experienced caregiver here, growing their skills, instead of leaving.
Laurie Bennett. Vice President of Human Resources at Sarasota (Fla.) Memorial Health Care System: We protected three non-negotiable priorities:
1. Employee engagement and recognition
We continued to invest in programs that reinforce appreciation and belonging, including: Annual service anniversary celebration, honoring milestone work anniversaries starting at five years up to 50 years; dinner program with entertainment and presentation of jeweled pins; monthly excellence recognition, with proclamation and award gifts; employee birthday cards, with coupons to spend at hospital eateries; food truck events, with free meals for all employees; and free tickets to seasonal circus, baseball and other community events.
These initiatives strengthen culture, connection, and retention of our highly skilled team members.
2. Growth and development: We expanded on- and off-site childcare and maintained our tuition reimbursement program, ensuring employees can learn, grow and build long-term careers within our system.
3. Retention of high-performing talent: With nearly 11,000 employees and a growing network of hospitals, specialty care centers and outpatient services, Sarasota Memorial is the region’s largest employer. By prioritizing engagement and development rather than short-term cost reductions, we supported stability across our workforce during a challenging financial environment.
Our commitment to people remains a strategic advantage — not an expense.
Lorina Wise. CHRO of Nationwide Children’s Hospital (Columbus, Ohio): Our continued investment in employee benefits reflects our hospital’s commitment to supporting our workforce. Over the past few years, we have reduced deductibles, minimized increases to employee premiums, and expanded our time-off programs — including PTO, caregiver leave and bereavement leave. We also remain focused on offering competitive wages, and have enhanced our employee assistance program to further support the emotional well-being of our staff and their families.
We continue to invest in events that celebrate our collaborative culture and honor the extraordinary dedication our employees demonstrate every day in caring for our patients and families. This includes employee recognition events, special traditions such as our holiday celebration and hospital birthday celebration, as well as targeted morale‑boosting activities and ongoing culture‑building initiatives. Together, these efforts help create an environment where our team can excel and deliver exceptional care.
Marc Boom, MD. President and CEO of Houston Methodist: Despite all the external turbulence facing healthcare, Houston Methodist is in an excellent financial position to withstand those headwinds. We steadfastly maintain our commitment to supporting our employees. We have robust programs where employees can pursue leadership training, ongoing clinical education and career development opportunities. We want our employees to maintain their purpose and passion for what they do because when they are fulfilled, patients benefit. Protecting these programs strengthens our culture and ensures that we continue providing high-quality patient care.
Mickey Foster. CEO of FirstHealth of the Carolinas (Pinehurst, N.C.): At a time when many healthcare organizations nationwide are facing margin pressure and rising labor costs, FirstHealth views investment in workforce well-being not as an expense, but as a strategic imperative. Supporting our team is essential to sustaining high-quality care for the communities we serve.
Through the Reid Center for Well-Being, we take a comprehensive approach to workforce development by supporting employees’ financial, physical, emotional, spiritual and community well-being. We offer robust retirement plans with matching contributions, on-demand pay through DailyPay and free fitness memberships for all employees. Our WellnessFirst program provides personalized health coaching and financial incentives for achieving wellness goals. Employees also have access to free, confidential counseling from a dedicated staff well-being team that also provides deployable wellness support across the organization.
From financial security, to fitness, to initiatives like partnering with Caring Hearts for Canines to bring adoptable dogs on-site, we are intentional about creating an environment where our team feels valued and supported. When we care for our people, they are better equipped to care for our patients — fulfilling our core purpose “To Care for People.”
Mitchell Rosner, MD. CEO of UVA Health and Executive Vice President for Health Affairs at the University of Virginia (Charlottesville): At UVA Health, workforce investment is not discretionary. It’s central to continuously delivering exceptional patient care and has been a core priority in our strategic plan for several years. Successfully recruiting, retaining, and developing our people is directly tied to patient safety and access and long-term stability, so our focus has been on building talent from within and aligning training with real care needs.
Even while facing margin pressure and rising labor costs, we protected and continued expanding programs that strengthen our workforce pipeline, from entry-level healthcare careers through leadership development. Our nationally recognized “earn while you learn” program provides paid, benefitted pathways into high-demand clinical and technical roles. These program graduates have filled hundreds of positions that have helped stabilize staffing in key areas. Parallel to that, our Health Leadership Institute prepares physicians, nurses, and operational leaders to lead increasingly complex health systems. Together, these efforts help us build a more stable workforce internally rather than relying solely on external hiring in a highly competitive market.
Myra Gregorian. Senior Vice President and Chief People and Transformation Officer at Seattle Children’s: At Seattle Children’s, we know that every person on our team — from our volunteers to our nurses and doctors — are a vital part of delivering healthcare. Despite the financial pressures facing healthcare today, we continue to make investments in our employees. We look at every workforce investment through the lens of our mission: providing hope, care and cures. This past year, we stood firm on investing in employee appreciation, competitive wages, mental health resources and comprehensive benefits, and technology that reduces administrative burden. When our team members feel seen and supported, they bring a level of empathy and excellence to our patients that is unmatched.
Tammy Peterman, MSN, RN. President of the Kansas City (Mo.) Division and Executive Vice President, COO and CNO at The University of Kansas Health System: More than 25 years ago, we developed our guiding formula to focus on quality, people and service. We believe when you have the best and right people supported in the best and right way, good things happen. Our quality outcomes and growth continue to show this is true.
At The University of Kansas Health System, we focus on culture and investment in our people, despite challenging economic conditions in healthcare. We created well-being programs designed to acknowledge the challenges of healthcare and to support mental and physical well-being. Our Employee Support After a Violent Event (E-SAVE) program is a Daisy Award winner for the team’s efforts to provide comprehensive resources to staff after a violent encounter. We have worked to provide additional meaningful benefits, including an additional discretionary holiday.
We created programs to invest in our team’s career development. Our GED program pays for school for eligible team members, gives them time during work hours for study and access to an executive mentor as they work toward a high school diploma. To support nursing, we have several programs including a nurse residency program, an ICU pathway program, and an ambulatory fellowship program. We have also provided a Thanksgiving gift card for all employees.
The post The workforce investments health system execs refuse to cut appeared first on Becker’s Hospital Review | Healthcare News & Analysis.
Telehealth costs 5 times less than office visits: Penn Medicine
Telehealth is about five times less expensive than in-office care for common conditions that can be treated by both types of visits, according to a new study from Philadelphia-based Penn Medicine.
The researchers analyzed over 160,000 visits — both virtual and in-person — billed to insurers across four months in 2024, focusing on 10 common conditions such as COVID-19, respiratory symptoms and anxiety. Initial telehealth visits were billed at an average of $400 less ($509 vs. $96 for in-office), and also resulted in fewer follow-up appointments (three vs. four), per the February study in JAMA Network Open.
Federal lawmakers recently extended pandemic-era telehealth flexibilities for Medicare beneficiaries, but only through 2027. Approximately 4-6% of healthcare visits are conducted virtually, another recent Penn Medicine study found.
“If telemedicine is allowed to revert to the more limited model that existed before COVID, the cost savings we identified could disappear,” said Kevin Mahoney, CEO of University of Pennsylvania Health System and a study co-author, in a Feb. 24 news release. “At a moment when hospitals and health systems face serious financial headwinds, those savings are vital. They enable us to reinvest in patient care and fuel innovation.”
The pricing gaps differed by condition, with telehealth visits for respiratory symptoms being about $800 cheaper on average and behavioral health costs roughly the same. The researchers noted that some of the in-person appointments were more serious and couldn’t be treated through telemedicine, but they adjusted their analysis to compare like patients across visit types as best they could.
The post Telehealth costs 5 times less than office visits: Penn Medicine appeared first on Becker’s Hospital Review | Healthcare News & Analysis.
How far are older adults patients willing to travel for care?: Study
Willingness among older adults to drive more than an hour for medical care varies by social demographics, according to a study published Feb. 23 in JAMA Network Open.
Researchers from Los Angeles-based University of Southern California surveyed 2,650 adults ages 65 and older through a nationwide internet-based survey called the Understanding America Study between April 23 and June 8.
Here are three things to know from the study:
- Among all survey respondents, the median willingness to travel times were:
- 67.5 minutes for primary care
- 127.5 minutes for specialty care
- 112.5 minutes for one-time diagnostic appointments
- The percentage of respondents willing to travel at least one hour to receive care were:
- 60.3% for primary care
- 84.4% for specialty care
- 82.5% for one-time diagnostic care
- Respondents willing to travel longer durations:
- Had higher incomes
- Greater educational attainment
- Were racial or ethnic minority individuals
- Typically drove themselves to appointments
Respondents unwilling to travel longer durations:
- Lived in metropolitan areas
- Reported being in fair or poor health
- Reported experiencing difficulty traveling for past medical appointments
Read the full study here.
The post How far are older adults patients willing to travel for care?: Study appeared first on Becker’s Hospital Review | Healthcare News & Analysis.
10 fastest-growing skills in healthcare
Workflow optimization is the fastest-growing skill in healthcare, according to a Feb. 24 LinkedIn News post.
LinkedIn News analyzed year-over-year growth in skills based on skill acquisition — the growth of a given skill being added to LinkedIn user profiles — and hiring success — the growth of a given skill possessed by users who have been hired in the past year. Growth rates were measured by comparing LinkedIn data from Dec. 1, 2024, to Nov. 30, 2025, with the same period in the year prior.
Here are the 10 fastest-growing skills in healthcare, per LinkedIn:
1. Workflow optimization
2. Cross-functional communication
3. Clinical monitoring
4. Standards compliance
5. Neurology nursing
6. Client relationship management
7. Clinical laboratory testing
8. Long-term care nursing
9. Nursing research
10. Report preparation
The post 10 fastest-growing skills in healthcare appeared first on Becker’s Hospital Review | Healthcare News & Analysis.
10 hardest-working US cities
Among U.S. cities, the hardest-working Americans live in Cheyenne, Wyo., according to an analysis by personal finance website WalletHub.
To determine the hardest-working cities, WalletHub compared 116 of the most populated cities across two dimensions, direct and indirect work factors. Analysts evaluated those dimensions using 11 metrics, ranging from average workweek hours to the share of residents who participate in local groups or organizations.
Each metric was graded on a 100-point scale, with 100 representing the hardest-working; cities’ weighted averages determined overall scores. More information about the methodology is available here.
Note: WalletHub used data from the U.S. Census Bureau, Bureau of Labor Statistics, U.S. Travel Association, Gallup, Social Science Research Council and Corporation for National & Community Service to create the ranking. Data for some metrics were only available at the state level.
The hardest-working cities in America, according to the analysis:
1. Cheyenne, Wyo.
2. Anchorage, Alaska
3. Washington, D.C.
4. Sioux Falls, S.D.
5. Irving, Texas
6. Nashville, Tenn.
7. Dallas
8. San Francisco
9. Denver
10. Austin, Texas
The cities at the bottom of the list, according to the analysis:
1. Burlington, Vt.
2. Detroit
3. Buffalo, N.Y.
4. Newark, N.J.
5. Toledo, Ohio
6. Bridgeport, Conn.
7. Columbia, S.C.
8. Providence, R.I.
9. Cleveland
10. Fresno, Calif.
The post 10 hardest-working US cities appeared first on Becker’s Hospital Review | Healthcare News & Analysis.
Private equity firm to acquire home health, hospice company in $1.1B deal — 5 things to know
Enhabit, a home health and hospice provider with 249 home health locations and 117 hospice locations across 34 states, has entered into a definitive agreement to be acquired by private equity firm Kinderhook Industries in an all-cash transaction valued at about $1.1 billion.
Five things to know:
1. Under the terms of the agreement, Enhabit stockholders will receive $13.80 per share in cash, representing a premium of about 24.4% to the company’s closing stock price Feb. 20, the last full trading day before the transaction was announced. The offer also reflects a 33.8% premium to Enhabit’s 60-day volume-weighted average share price for the period ended Feb. 20.
2. Upon completion of the transaction, Enhabit’s common stock will no longer be listed on the New York Stock Exchange and the company will become privately held. Enhabit will continue operating under its existing name and brand.
3. The acquisition was unanimously approved by Enhabit’s board of directors and is expected to close in the second quarter, subject to stockholder approval, regulatory approvals and other closing conditions. Certain Enhabit executive officers have entered into voting and support agreements to vote in favor of the transaction at a special meeting of stockholders.
4. Barb Jacobsmeyer, president and CEO of Enhabit, said the transaction positions the company for long-term growth. “Under Kinderhook’s ownership, Enhabit will benefit from additional resources and expertise that will support long-term investments in our people, clinical excellence and innovation without the short-term pressures of the public markets,” Ms. Jacobsmeyer said in a Feb. 23 news release.
5. New York City-based Kinderhook focuses on middle market businesses in healthcare services, environmental and industrial services, and light manufacturing and automotive sectors. The firm has raised more than $10 billion in committed capital and has completed more than 500 investments and follow-on acquisitions.
The post Private equity firm to acquire home health, hospice company in $1.1B deal — 5 things to know appeared first on Becker’s Hospital Review | Healthcare News & Analysis.
States with the most top home health programs: US News
California has the most top-rated home health programs, according to U.S. News and World Report’s inaugural ranking. Three states and Washington, D.C., do not have any.
U.S. News evaluated more than 12,000 Medicare-certified home health agencies across the country using CMS data. Home health programs were rated based on quality and patient experience measures, including timely initiation of care and outcomes, and preventable hospitalizations. To be eligible for rating, home health agencies had to have a CMS certification number, and reported quality of patient care star rating, patient survey rating or both. U.S. News used an independent methodology, resulting in some of its ratings differing from the CMS rating program. Read more about the methodology here.
Just over 1%, or 1,319, of home health agencies earned the Best Home Health distinction for exceeding expectations in care quality and patient experience. Agencies with this designation began care on time for 99% of patients, compared to the national average of 94%. Among patients in top-rated agencies, 93% saw an improvement in walking and moving, compared to 83% nationwide. These patients were also more likely to get better at getting out of bed, bathing themselves and taking medications correctly.
Here are the states ranked by how many top-rated home health agencies they have:
California: 151
Texas: 133
Florida: 105
Louisiana: 77
Alabama: 73
Tennessee: 62
Illinois: 61
Pennsylvania: 53
North Carolina: 50
Ohio: 50
Kentucky: 44
Oklahoma: 39
Missouri: 38
Michigan: 34
Arkansas: 33
South Carolina: 32
Indiana: 30
Virginia: 29
Mississippi: 28
Massachusetts: 27
Georgia: 26
Wisconsin: 22
Minnesota: 21
New York: 21
West Virginia: 21
Arizona: 20
Iowa: 19
Colorado: 18
Kansas: 17
New Mexico: 15
Utah: 14
South Dakota: 12
Maryland: 11
Idaho: 10
Nevada: 9
New Jersey: 8
Maine: 7
Delaware: 6
New Hampshire: 6
Rhode Island: 6
Connecticut: 5
Nebraska: 5
Washington: 5
Oregon: 4
Wyoming: 3
North Dakota: 2
Hawaii: 1
Alaska: 0
District of Columbia: 0
Montana: 0
Vermont: 0
The post States with the most top home health programs: US News appeared first on Becker’s Hospital Review | Healthcare News & Analysis.
‘Think of your hospital as a startup’: What Mark Cuban would do if he bought a hospital
If Mark Cuban bought a hospital, he says he would run it like a startup: eliminate unnecessary overhead, prioritize radical transparency, pay physicians well and use AI to root out inefficiencies.
Speaking on “The Healthcare Bridge” podcast with Nathan Kaufman, managing director and founder of Kaufman Strategic Advisors, Mr. Cuban — co-founder of Cost Plus Drugs Co. — discussed how he believes hospitals could be operated differently.
“You’ve got to be able to get down like any other startup,” he said. “You’ve got to think of your hospital as a startup, and your first doctors as your first employees or your partners.”
Mr. Cuban questioned traditional hospital cost structures, pointing to what he sees as unnecessary spending.
He said he would design a hospital with minimal overhead: no lavish amenities, fewer consultants and no unnecessary administrative layers. Instead, he suggested a lean model that avoids expensive infrastructure, relies on essential technology and outsources services when necessary.
The foundation of his approach would focus on simplifying operations, eliminating ancillary services and building trust.
“It is the same with Cost Plus Drugs. Our margins are only 15% but I know that the key element for me is how I build trust, and the way to build trust is by having a set margin,” Mr. Cuban said. “If I did buy a hospital … I would get rid of all the ancillaries and market it much like we do Cost Plus Drugs and pay my doctors more. We don’t have many employees, but we pay them well.”
Transparency would also be critical to the model. Rather than treating pricing and physician compensation as confidential business information, he argues that making the hospital’s costs and reimbursements fully visible would offer it a competitive advantage.
“I would put out there and market, look, here’s what we pay our doctors. Here’s our overhead — down to the penny — so that you can see what it costs. And here’s what we get reimbursed by Medicare, and we’ll charge you the same, and we’ll grow,” he said. “I know that practice would grow, because even though basic Medicare doesn’t make you much money, the people who have real issues, you can make money from.”
He framed hospital economics as largely dependent on market leverage, arguing hospitals typically fall into one of two categories. In his view, negotiating power — not necessarily operational efficiency — often determines financial success.
“One, I have market dominance, and I get to say, ‘f— you,’ to everybody and the insurance companies, right? I don’t need you, because I’m going to get my own patients too,” Mr. Cuban said. “Two, I don’t have enough patient flow, so I need you insurance companies to send me patients, and so I’ll do the deal that you want me to do, because otherwise I don’t have a patient funnel.”
He also argued that hospital executive incentives often drive expansion for scale rather than long-term sustainability.
“I think part of the challenge is [how] most CEOs are rewarded. Hospital CEOs are rewarded by revenues and scale, and so they default to more buildings,” he said. “If this 100-bed hospital is not my final destination, I want to be the 60-hospital, 6 zillion beds, because that’s where I’m making $10 million a year.”
Mr. Kaufman noted that consolidation can provide negotiating leverage with payers but cautioned that scale alone is insufficient.
“If you have beds [but] insurance companies aren’t paying anything, you have no negotiating cloud at all,” Mr. Kaufman said. “So you do need to consolidate to get big, but you have to know how to run that business.”
Mr. Cuban pointed to AI as a major opportunity, particularly in contract and revenue oversight.
“One of my clients just acquired a 250-bed hospital. It was bankrupt, owned by a [private equity] firm, but that hospital had over 3,000 contracts,” Mr. Kaufman said. “That’s not a 600-bed hospital. It’s a 250-bed private hospital, so that just gives you some idea of the magnitude of management that needs to occur.”
Mr. Cuban said automation could quickly and effectively solve that complexity.
“Imagine all those processes associated with all those contracts could be automated with AI agents, because there’s nobody verifying all the financial information associated with transactions from each one of those contracts,” he said. “No chance you can’t hire enough people to do that.
“That’s what agentic AI is really going to do for hospitals and clinics and practices’ low hanging fruit.”
Ultimately, Mr. Cuban said his approach would center on a simple entrepreneurial question.
“I put my entrepreneur ‘Shark Tank’ hat on … [and ask], ‘What would it take to get people to choose me?’”
Click here to listen to the full episode of the podcast.
The post ‘Think of your hospital as a startup’: What Mark Cuban would do if he bought a hospital appeared first on Becker’s Hospital Review | Healthcare News & Analysis.
‘The best ideas come from the front lines’: Why Penn State Health’s CEO still practices medicine
When Michael Kupferman, MD, became CEO of Hershey, Pa.-based Penn State Health in late June 2025, he brought a special background that not all health system executives have: decades of work as a physician.
Dr. Kupferman began practicing medicine in 1999, and is a trained head and neck surgeon. In his new role, he works with clinical colleagues one to two days monthly while maintaining his CEO responsibilities.
“It keeps me grounded being able to be part of day-to-day patient care,” Dr. Kupferman told Becker’s. “It’s what I’ve always loved to do. It’s why I became a physician. Even though I don’t get to spend as much time with patients directly, I feel like my role is to empower our caregivers to do their best work so that they can provide exceptional patient care.”
Dr. Kupferman also splits his time across Penn State Health’s hospitals and clinics each week, meeting with colleagues, patients and their families. It’s through these interactions that he is able to more deeply understand any pain points at the system and address them accordingly.
“The best ideas come from the front lines, [they don’t] come from the C-suite,” he said. “The best initiatives, the most foundational ideas really come from our physicians, our nurses and our team members. They’re the ones who we engage with in this process.”
Along with creating a strong front-line presence with employees, Dr. Kupferman is also leading Penn State Health through an Epic integration to improve clinician and patient experience.
The six-hospital system began implementation of the new EHR in June, and plans to go live with it in the fourth quarter of 2026.
“Everything’s going quite well,” Dr. Kupferman said. “We are making the hard decisions around systemness, and that’s what the Epic implementation entails. Bringing the broad array of stakeholders together to align around how, for example, our laboratories are going to run, how our imaging centers are going to run, how we’re going to manage our operating rooms and what that patient experience looks like when they check in at the front door.”
Penn State Health is also working to integrate its academic and community physicians into a single unified medical group, further cementing its identity as the only integrated academic health system in the region.
“We cover the entire waterfront,” he said. “The integrated medical group creating systemness is going to enhance that exceptional patient experience, that exceptional patient access that we continue to promise and deliver in this region.”
The post ‘The best ideas come from the front lines’: Why Penn State Health’s CEO still practices medicine appeared first on Becker’s Hospital Review | Healthcare News & Analysis.
3 big questions surrounding the Rural Health Transformation Program
As funds begin flowing to states through the five-year, $50 billion Rural Health Transformation Program, hospital leaders are confronting a central question: Will the initiative meaningfully stabilize struggling providers — or will it fall short of offsetting an estimated $137 billion in Medicaid cuts to rural communities over the next decade?
The program, enacted in July as part of HR1, is designed to support broader health system transformation in rural areas. But its structure — including limits on direct patient-care payments and significant state discretion — has raised uncertainty about how much the program will ultimately benefit rural hospitals.
Here are three major questions surrounding the program:
1. How much will rural hospitals actually receive?
Unlike previous federal relief programs, this one does not provide direct payments to rural hospitals. Instead, states applied for and are managing the funds. States are not legally required to allocate money to rural hospitals specifically.
CMS stipulates that direct payments to hospitals and other providers for patient care cannot exceed 15% of total funds, though providers could benefit through other means, such as infrastructure investments (capped at 20%).
State applications varied in detail, but common themes emerged, such as workforce development, telehealth, partnerships and network development, interoperability, and preventive measures promoting healthier lifestyles, according to Chartis.
KFF said in a January report that it is unclear how much of the money will benefit rural hospitals either directly or indirectly and the extent to which this will offset hospitals’ losses under the reconciliation bill.
Damond Boatwright, CEO of Springfield, Ill.-based Hospital Sisters Health System, sees the program as a significant opportunity to reverse the long decline of rural healthcare, but the majority of the funds must flow directly to rural providers and not be diverted toward nonclinical or private equity and venture capital-backed enterprises.
“The majority of RHT funds must reach rural providers who deliver care, sustain access and anchor their communities,” Mr. Boatwright recently wrote for Becker’s. “Strengthening rural hospitals, clinics and caregivers — while simultaneously investing in workforce development, broadband, economic revitalization, transportation and social determinants — creates a resilient ecosystem where rural Americans can thrive.”
The sentiment is shared by Texas Hospital Association President and CEO John Hawkins.
“The proof will be in the details,” he said in a statement shared with Becker’s. “The dollars need to be focused on hospitals, which took the brunt of the Medicaid cuts. They need to come quickly without unnecessary administrative hurdles. They need to be self-sustaining, flexible and not create new burdens.”
2. What will future funding rounds look like?
When CMS announced the first-year funding amounts in December, variation in funding per-state was relatively narrow. Texas received the most first-year funding with $281.3 million and New Jersey received the least with $147.3 million.
Half of the program’s funds are being distributed equally to each state, meaning that $100 million is allocated from 2026 through 2030 to all 50 states. The other half involves a formula that factors in a state’s rural score — which considers rural population, number of facilities, land area and the share of hospitals receiving disproportionate share hospital payments — as well as technical scoring for project proposals, KFF News reported Jan. 14.
Texas’ first-year funding includes $105.1 million in rural funding and $76.2 million in technical funding, according to KFF News’ analysis of data from the University of North Carolina’s Cecil G. Sheps Center for Health Services Research. New Jersey’s rural funding was $22.8 million and its technical funding was $24.5 million.
Mark Holmes, director of the Cecil G. Sheps Center for Health Services Research, told KFF News that the technical score is a crucial consideration because those funds can be redistributed and potentially clawed back in future years.
“We can be fairly certain that every state will get at least a slightly, if not a vastly, different amount next year based on this re-pooling and reallocation piece,” Mr. Holmes told the news outlet.
3. Can struggling rural hospitals keep their doors open?
Forty-one percent of rural hospitals are operating at a loss and 417 are vulnerable to closure, according to a Feb. 10 report from Chartis.
Chartis said that while state initiatives have the opportunity to positively affect healthcare in rural communities, the program may be too late to prevent more hospitals from closing their doors or removing service lines. Since 2010, there have been 206 rural hospitals that have either closed or converted to models that exclude inpatient care, such as the Rural Emergency Hospital Model.
The firm’s analysis found that more than 10 million rural Americans rely on Medicaid. At the median rural hospital, Medicaid represents nearly 10% of total revenue. Chartis said the Medicaid-related cuts outlined “will severely impact cash-strapped rural hospitals.”
“The Medicaid cuts that take effect in 2027 will intensify efforts to stabilize the financial viability of rural hospitals,” Chartis said. “Rural hospitals need to plan for those cuts while using RHT funding at the state level to deliver the maximum benefit from those programs and initiatives to the communities they serve.”
The post 3 big questions surrounding the Rural Health Transformation Program appeared first on Becker’s Hospital Review | Healthcare News & Analysis.
Healthcare wage growth weakens: Indeed
Healthcare wage growth weakened in the six months leading up to December across most categories analyzed, according to a Feb. 20 research brief from Indeed’s Hiring Lab.
Here are six things to know from the fourth-quarter healthcare labor market update:
1. Wage growth in most healthcare categories — including personal care and home health, dental, childcare and therapy — exceeded the overall labor market average of 2.1% in December, based on year-over-year, three-month average posted wages on Indeed. Medical technician and nursing roles fell below the overall average, at 2% and 1.2%, respectively.
2. All categories in the report saw declining wage growth in the six months leading up to December, except dental, which remained flat. Over that period, wage growth declined by 1.2 percentage points for medical technicians and 0.9 percentage points for nursing roles.
3. In the fourth quarter of 2025, Indeed job posts fluctuated between 2% and 6% above its Feb. 1, 2020, baseline. As of Jan. 23, U.S. job postings were 4.4% above the pre-pandemic baseline and had declined 5.9% from Jan. 23, 2025.
4. As of Jan. 23, 2026, therapy and physicians and surgeons roles were up 88.4% and 84.1%, respectively, from the Feb. 1, 2020, baseline. Year over year, those categories were down 0.5% and 0.9%, respectively.
5. Pharmacy was the only category with increased job postings over the past year, up 4.2%, and postings were 27.6% above the Feb. 1, 2020, baseline. Medical technician roles were down 9.3% year over year and remained 23.7% above the pre-pandemic baseline.
6. Nursing job postings were down 9.8% year over year and were 7.6% above the Feb. 1, 2020, baseline.
The post Healthcare wage growth weakens: Indeed appeared first on Becker’s Hospital Review | Healthcare News & Analysis.
South Carolina measles admissions ‘vastly underreported’: ProPublica — 3 updates
Medical experts believe measles-related hospitalizations in South Carolina are significantly higher than reported, since the state does not require hospitals to report admissions for the virus, ProPublica reported Feb. 20.
South Carolina is experiencing the nation’s largest measles outbreak since the virus was declared eliminated in 2000. More than 970 cases have been confirmed in the state since late October, the majority of which have occurred among unvaccinated individuals, according to data from the state’s health department.
Hospitals in the state have reported 20 measles-related admissions since the outbreak began in the fall, indicating a 2% hospitalization rate. That is likely a significant undercount, with only a handful of hospitals in regions affected by the outbreak having reported hospitalizations, experts told the news outlet.
“A hospitalization rate at 2% is ludicrous,” Paul Offit, MD, an infectious disease physician and director of the Vaccine Education Center at Children’s Hospital of Philadelphia, told ProPublica. “It’s vast underreporting,” he said. “Measles makes you sick.”
Officials with the state health department are urging hospitals to report all measles-related admissions, though cannot force them to do so. The Department of Public Health said it has not added hospitalizations as a reporting requirement for infectious diseases since the primary purpose of public health surveillance is to understand transmission patterns, rather than track complications.
However, physicians say not having an accurate picture of hospitalizations and complications can make the outbreak appear less severe than it is and hinder efforts to clearly communicate the risks to the public, particularly for young children and unvaccinated individuals.
“It’s a very big disservice to the public not reporting complications we are seeing in hospitals or even ERs,” Leigh Bragg, MD, a pediatrician in South Carolina, told ProPublica.
Three more updates on measles outbreaks in the U.S.:
1. Less than two months into the year, case counts are already nearing 1,000. As of Feb. 19, there have been at least 982 confirmed cases of measles in the U.S., according to the latest CDC data. At the current pace, 2026 could far outpace 2025, when 2,280 cases were reported nationwide for the full year.
2. South Carolina has been the hardest hit, with 632 cases confirmed so far this year, according to CDC data. Overall, 26 states have reported measles cases in 2026. Outbreaks are also growing in Utah, Florida and Arizona.
3. As measles outbreaks expand, more hospitals are grappling with exposure incidents, triggering infection prevention protocols and public health notifications. In recent weeks, facilities in Oregon, North Carolina, the District of Columbia, New Jersey, Utah and South Carolina have been identified by state and local health departments as potential exposure sites.
The post South Carolina measles admissions ‘vastly underreported’: ProPublica — 3 updates appeared first on Becker’s Hospital Review | Healthcare News & Analysis.
How health systems are tackling behavioral health fragmentation
Health systems are responding to fragmented behavioral healthcare delivery in different ways: expanding telepsychiatry in rural states, building pediatric health hubs that integrate mental and physical health on one campus, launching behavioral health urgent cares, and investing in navigators and data infrastructure to keep patients connected after discharge.
In West Virginia, the access challenge is especially stark.
Keri Law, MD, a child and adolescent psychiatrist and vice chair of clinical services at WVU Medicine in Morgantown, W.Va., told Becker’s that 50 of 55 counties are federally designated mental health professional shortage areas. As a result, some families must travel two to four hours for specialty behavioral healthcare — if it is available at all.
Over the last three years, virtual care has become a critical strategy for improving access.
“In terms of just our volumes, the number of total patient visits that we’re seeing virtually in our clinic, within the department of behavioral medicine and psychiatry, are still lingering a little over 50%,” she said. “And that’s with having about 100,000 patients per year, and with kids they’re a little bit less, but still at around a third of our children are seen virtually.”
Dr. Law said virtual visits have helped improve access, shorten time to first appointment, and strengthen continuity of care, particularly for pediatric patients and those in remote areas. No-show rates are often lower for virtual visits, especially in rural populations, where transportation and weather can be major barriers, she said.
Building shared data networks
At the national level, children’s hospitals are also collaborating to address fragmentation through shared data and infrastructure.
A behavioral health leadership collaborative within the Children’s Hospital Association has joined forces with a youth suicide prevention initiative to form a network of 30 hospitals focused on the advancement of pediatric behavioral health through data-sharing and evidence-based models, Stacy Drury, MD, PhD, psychiatrist-in-chief at Boston Children’s, told Becker’s.
Fragmented data is a common challenge in behavioral health. By connecting systems and standardizing processes, hospitals can avoid building programs in silos.
For example Columbus, Ohio-based Nationwide Children’s operates its own behavioral health transport to more efficiently transfer children from the emergency department to inpatient care.
“[Nationwide Children’s] had all of the policies and procedures already in place,” Dr. Drury said. “They knew how to make the car, and they built it again at Cincinnati Children’s, so now we have one and there’s another one on the north shore in Boston.’”
EMR integration to bridge physical and mental healthcare
At Cincinnati Children’s, leaders are also working to decrease barriers between physical and mental healthcare through data integration, Laurel Leslie, MD, director of the hospital’s mental and behavioral health institute, told Becker’s.
“We’ve found a way for outpatient mental health providers that are not in [Cincinnati] Children’s to be able to link into our EMR, and then they can track if kids have come into the emergency department, if they’ve been hospitalized,” she said. “We can also see if they have openings available.”
In addition to improving coordination through data, some systems are investing in physical integration.
Boston Children’s Hospital is developing a $640 million pediatric psychiatric hospital on Franciscan Children’s campus aimed at integrating mental health across pediatric medicine, Stacy Drury, MD, PhD, psychiatrist-in-chief, told Becker’s.
The project will include 116 inpatient beds and a day hospital with 24 slots for partial hospitalization and intensive outpatient programs, as well as a 14-bedroom, community-based acute treatment program. The building will house a dental suite, a surgical suite with four operating rooms and 10 preparatory and post-recovery slots, a pharmacy and an outpatient rehabilitation space.
Patients and their families are able to shift between partial-hospitalization programs and outpatient services or connect with a higher level of care, she said.
“To have that capacity in the same building is huge. Families don’t have to choose between getting their dental care and getting their mental healthcare,” Dr. Drury said. “I think being very intentional about the medical complexity kids with neurodevelopmental disorders really need to be within the same place.”
Providing navigators to support patients after discharge
Health systems are also addressing fragmentation in the transition from acute care to the community.
Behavioral health and substance use navigators connect patients to aftercare services following discharge from the emergency department — a point at which many patients disengage from care, Itai Danovitch, MD, chair of the department of psychiatry and behavioral neurosciences at Los Angeles-based Cedars-Sinai Medical Center, told Becker’s.
Navigators help link patients to the resources they need to remain connected to substance use disorder services and their communities. They do not provide psychotherapy. Instead, they serve as nonclinical, peer-based supporters focused on engagement and trust building.
“It takes time to engage a patient who’s been traumatized, or feels stigmatized or embarrassed and ashamed of some of their behaviors,” Dr. Danovitch said. “These are roles that can help with some of the soft skills that are so important to engaging individuals who have had negative experiences with hospitals in the past.”
Strengthening the health system workforce pipeline
Fragmentation also exists within health system workforces.
New York City-based NYC Health + Hospitals, the largest provider of behavioral health services in the city, has focused on closing gaps in its behavioral health workforce through a strategic recruitment and retainment plan. With 11 acute care facilities and more than 30 community health centers, fragmentation can happen at both the departmental and system levels.
When human resources, finance and program leadership are not aligned, initiatives can stall and responsibilities can fall between departments, Omar Fattal, MD, system chief of behavioral health, told Becker’s. Fragmentation can also emerge between individual facilities and system leadership.
To address this, the system brought leaders together around a shared strategic plan, aligning objectives and preparing departments for upcoming changes.
“What we’ve done is really centralized the scaffolding, support and structure, but not the people, in the sense that we definitely standardized data,” Dr. Fattal said. “You cannot do this work without data. You cannot fly this plane completely blind. And you really need to know how many vacancies you have. For every program that we have, you have to keep track of, ‘Is it working? Is it not working?’”
The system has since adopted a data infrastructure that tracks programs, vacancies and open positions to better support retention and workforce planning.
Another strategy to reduce fragmentation is diverting appropriate patients away from the emergency department.
St. Louis-based SSM Health has adopted a behavioral health urgent care separate from the emergency department. The facility is staffed by psychiatric nurse practitioners, nurses and social workers, and provides care for patients who have run out of medication or could not secure a timely psychiatrist appointment, Becky Dvorak, MSN, RN, regional vice president of behavioral health, told Becker’s.
“Getting into a psychiatrist could take months,” she said. “This helps meet the need early on instead of waiting four months and turning it into a crisis that ends up in the hospital.”
The system is working to ensure EMS providers are comfortable transporting patients directly to the urgent care rather than the emergency department. Through county grants, EMS providers can be reimbursed for transporting certain patients to urgent care, helping support the shift in care pathways.
The post How health systems are tackling behavioral health fragmentation appeared first on Becker’s Hospital Review | Healthcare News & Analysis.
Historic New York City nurses strike ends after 41 days
The largest nurses strike in New York City has ended after 41 days, with the final group of striking nurses voting to ratify a contract with NewYork-Presbyterian.
The final group of nurses voted Feb. 21 to ratify a new three-year contract and began returning to work Feb. 23, according to a news release from the New York State Nurses Association. The group of approximately 4,200 nurses reached a tentative agreement Feb. 19.
“We are pleased to share that we have a new ratified contract with the New York State Nurses Association and look forward to our nurses’ return to the hospital,” a NewYork-Presbyterian spokesperson said in a Feb. 21 statement shared with Becker’s. “The new contract reflects our respect for our nurses and the critical role they play as part of our exceptional care teams.”
Approximately 15,000 nurses went on strike Jan. 12 at Montefiore Health System, Mount Sinai Health System and NewYork-Presbyterian. Nurses at Montefiore and Mount Sinai reached tentative agreements Feb. 9 and ratified them Feb. 11.
The ratified contracts feature salary increases of more than 12% over the three-year deals, improved safe staffing standards, protections to healthcare benefits and safeguards against artificial intelligence. They also include protections from workplace violence and protections for immigrant patients and nurses, the release said.
“We are so happy with the wins we achieved, and now the fight to enforce these contracts and hold our employers accountable begins,” NYSNA President Nancy Hagans, BSN, RN, said in the news release. “NYSNA nurses showed what it means to advocate for patients, and this moment will go down in history as a win for our communities, in the fight for healthcare justice, and for the labor movement.”
The post Historic New York City nurses strike ends after 41 days appeared first on Becker’s Hospital Review | Healthcare News & Analysis.
6 lessons shaping health system strategic leaders’ operational approach for 2026
Challenges such as emerging technology, government regulations, workforce shortages and increasing labor costs have driven a number of health system strategic leaders to pivot their approach for 2026.
Faced with these challenges, leaders are creating new ways to empower frontline staff and upgrade patient care while trying to increase system efficiency and profit margins.
Becker’s asked six health system strategic leaders about the leadership lessons that shaped their operational approach for this year.
If you are a COO or strategic leader in healthcare and are interested in joining Becker’s Healthcare COO + Strategic Leader virtual community, please contact Scott King at sking@beckershealthcare.com.
Editor’s note: Responses have been lightly edited for clarity and length.
Question: What leadership lesson has shaped your operational approach for 2026?
Bryan Croft. Executive Vice President and COO, Cedars-Sinai Medical Center (Los Angeles): Given the operational challenges facing healthcare, I would advise leaders to get out of your office and walk the halls. See and talk to patients. See and talk to your people, your caregivers and get to know what motivates them to come in and deliver care, and help your institution put its best foot forward. I think you will find it not only rewarding but it will help ground you in the sacred mission of helping people navigate some of the most trying times of their lives.
Brian Evans. CEO, Optim Health System (Savannah, Ga.): “Control what you can control.” It’s advice I’ve heard time and time again. But with shifting payer mixes and the rising costs of labor and supplies, margin goals are increasingly difficult to reach. In 2026, my focus is sharp: I am prioritizing the variables within my scope to cut costs, maximize efficiency and aggressively drive revenue.
Dawn Thompson. Chief Strategy Officer, Advanced Diagnostics Healthcare System (Houston): Healthcare operations improve when leaders design systems that make the right thing the easy thing to do. Operations must be designed around systems — not individual heroics.
Doug McGill. Vice President of Quality Strategy and Operations, Emory Healthcare (Atlanta): One leadership lesson stands out most for me: strategy only creates value when it shows up reliably at the frontline of care. Emory Healthcare’s new tagline, “The frontline of care. The forefront of discovery,” captures that tension well. Discovery and strategy matter, but they only make a difference when they are translated into consistent, executable practice.
That belief has shaped my operational approach for 2026. Advisory influence alone isn’t sufficient. The work has to be embedded through clear standards, empowered accountability and dependable data so that high performance is designed into everyday operations, not reliant on extraordinary effort to overcome system gaps. That’s how we’ll lead well and transform care delivery – by making excellence reliable at the frontline.
Matthew Timmons. COO, LCMC Health (New Orleans): As our senior leadership team was developing goals and priorities for 2026, a clear theme arose from our discussions: meaningful and intentional prioritization. As we have now moved into the first part of the year, our approach is being driven by a clear, narrowed focus on a smaller number of priorities. Instead of spreading out our effort across a laundry list of organizational needs, we have prioritized our initiatives around patient care, patient and team experience, and long-term access and growth. We are confident this approach will enable us to align our actions and energy, which will ensure we achieve extremely successful and sustainable results.
Kelli Novant. Executive Vice President, Chief Legal Officer, Novant Health (Winston-Salem, N.C.): My operational approach for 2026 is fundamentally shaped by the understanding that how I engage my team matters as much as the decisions I make. I’m focused on fostering collaborative, candid conversations that build trust and encourage thoughtful dialogue. By modeling openness and inviting feedback, I help create a culture that brings forward multiple perspectives, leading to more well‑rounded recommendations and decisions. Building and maintaining trust – both within my team and across the organization – is essential because investing in people and relationships leads to stronger decision‑making and more sustainable long‑term outcomes.
The post 6 lessons shaping health system strategic leaders’ operational approach for 2026 appeared first on Becker’s Hospital Review | Healthcare News & Analysis.
The ‘uncomfortable decisions’ ahead for hospital CFOs
The hardest work ahead for CFOs isn’t finding opportunities for growth. It’s narrowing them.
In a recent conversation with “Becker’s Healthcare Podcast,” Sophia Holder, executive vice president and CFO of Children’s Hospital of Philadelphia, described the next phase of leadership as one defined by discipline and discomfort.
“Our hardest work ahead is continuing to make disciplined and really sometimes uncomfortable decisions while staying grounded and anchored in our mission,” she said. “That includes likely saying no to investments that do not clearly advance access, quality and sustainability, and pushing ourselves to rethink legacy structures and our ways of working.”
Many finance leaders are confronting a similar balance between team performance in the near-term and long-term capability building. Headwinds including labor shortages, increasing costs and reimbursement pressure are making a huge impact on hospitals’ bottom lines, while the dearth of technology and AI-driven platforms can easily become expensive solutions in search of a problem.
“We are in an increasingly complex healthcare landscape. How do we grow and innovate in a sustainable way?” Ms. Holder said. “For us, this means having more honest conversations, making really clear choices, really tuning into our prioritization framework and aligning our resources with what matters most for children and families. The result was not only to improve financial performance, which I was really grateful for as CFO, but create stronger organizational alignment and a clear connection between the financial decisions and patient impact.”
Hospital C-suite executives are accountable for balancing near term performance with long-term capacity building. Given the uncertainties in healthcare today, many are taking a more conservative approach and forgoing investments they may have made in the past, even if those investments have marginal returns.
“We are focused on sustaining financial performance in an environment of continued labor pressures, reimbursement dynamics and ongoing volatility in volumes,” she said. “At the same time, we are prioritizing long term capability building.”
That includes workforce optimization, revenue cycle resilience and capital discipline. It also means the leadership team is zeroing on responsible deployment of automation and AI to reduce administrative burden and improve data-driven decision-making.
“The challenge is balancing near term performance with these longer term investments so that we do not compromise access, do not compromise growth in our longer strategic objectives, or we do not compromise innovation for children and families,” she said.
CHOP’s leadership team has a strong growth mindset and sees the best opportunities at the intersection of mission and discipline, Ms. Holder said. In the coming year, the organization plans to expand access through ambulatory and virtual models, strengthen partnerships regionally, nationally and internationally, and add services that will differentiate outcomes for patients.
Internally, growth means adding capabilities and developing leaders.
“We are focused on modernizing our operating models, and as the CFO, we are also focused on embedding this notion of financial stewardship into everyday decision making,” said Ms. Holder. “It’s not a one-off; it’s ingrained in our culture. When we do that well, growth becomes sustainable, not just bigger. We’re not just bigger, but stronger. This is an exciting time for us at CHOP, ripe with opportunities despite the changes that are surrounding the entire healthcare landscape.”
The post The ‘uncomfortable decisions’ ahead for hospital CFOs appeared first on Becker’s Hospital Review | Healthcare News & Analysis.
Medicare Advantage’s ‘sunk-cost’ problem
Medicare Advantage now covers about 55% of eligible beneficiaries nationwide — more than 35 million people — but health systems are confronting a question that until recently felt almost taboo: What happens when participation in the country’s fastest-growing Medicare program no longer makes financial sense?
Over the past three years, Becker’s has reported on roughly 90 hospitals and health systems that have terminated some or all of their commercial Medicare Advantage contracts. In 2026 alone, at least 15 systems have gone out of network with one or more Medicare Advantage plans, and the trend is showing no signs of slowing down.
This year, 1 in 10 Medicare Advantage enrollees — about 2.9 million people — will be forced to disenroll from their plan following a spike in plans exiting the market, according to a Feb. 18 study published in JAMA.
Behind many of those decisions lies what Scripps Health CFO Brett Tande describes as a classic “sunk-cost” dilemma: after years of building infrastructure, staffing and strategy around Medicare Advantage, can systems realistically walk away — even when contracts are losing money?
For a growing number of health systems, the answer is becoming clearer.
Becker’s connected with executives from Providence, Scripps Health, Ascension, MemorialCare and Mayo Clinic to understand how they are reassessing their participation in Medicare Advantage and what that shift could mean for providers, payers and patients.
When the math no longer works
San Diego-based Scripps Health made headlines Jan. 1, 2024, when it exited nearly all of its commercial Medicare Advantage contracts, affecting roughly 32,000 beneficiaries across five health plans.
“It was a tough decision to make,” Scripps President and CEO Chris Van Gorder told Becker’s. “But we were losing about $75 million a year on those contracts, and the payers weren’t willing to negotiate the changes we needed — not just higher reimbursement, but addressing prior authorization issues and paying us what they were contractually obligated to pay.”
More than two years later, executives say the decision paid off.
Since exiting Medicare Advantage, Scripps has not reported a quarterly loss, according to Mr. Tande. Ratings agencies that downgraded Scripps in late 2023 have since signaled potential upgrades. While there was some ambulatory volume softness, inpatient volumes largely held steady. Many patients ultimately switched back to traditional Medicare with a supplemental plan to maintain access.
“A lot of things have changed since then,” Mr. Tande said. “But that’s an important data point.”
Scripps’ experience challenges a core assumption underpinning many systems’ Medicare Advantage strategies: that exiting contracts will trigger catastrophic volume loss. For systems with strong market positions, that risk may be less severe than feared.
But not every organization has Scripps’ leverage.
“For the average hospital, that’s a much scarier proposition,” Mr. Tande said. “But I still think you’re going to see more systems exit, because continuing to absorb losses isn’t sustainable. At some point, the decision has to change.”
The structural flaw providers underestimated
Beyond individual contract disputes, some leaders argue that Medicare Advantage has a structural flaw that providers have long underestimated.
“Insurance is actually a low-margin business,” Mr. Tande said, citing public filings from national payers. “Medicare Advantage insurance is, at best, a 2% to 3% margin business — and that’s when you run it with prior auth and other practices many of us find caustic.”
The more profitable segments for diversified insurers often lie in adjacent businesses — pharmacy benefit management, physician services or analytics subsidiaries — rather than in the Medicare Advantage insurance product itself.
Health systems, by contrast, lack the national scale and diversified revenue streams to subsidize thin Medicare Advantage margins, according to Mr. Tande.
“One of the reasons health systems got into MA was to gain market share,” he said. “But you can’t make money on traditional Medicare, and you certainly can’t make money on Medicare Advantage, which ultimately pays less. Yet systems have built very expensive infrastructure around MA and are afraid that if they exit, volume will go elsewhere.”
That dynamic — heavy upfront investment combined with fear of losing patients — creates what he calls a “sunk-cost fallacy.”
“Organizations have positioned themselves so they feel they have to keep hospitals full — and they’re doing it with MA payers that are terrible,” he said. “They’re stuck between two bad decisions.”
Providence CEO calls for a Medicare Advantage ‘reset’
Renton, Wash.-based Providence has not exited Medicare Advantage wholesale, but it has taken a firmer stance in negotiations. Last month, Providence Clinical Network — which includes 15 hospitals in California — went out of network with UnitedHealthcare MA.
Erik Wexler, president and CEO of Providence, called for a broader “reset” of the program in a January interview with Becker’s.
“If we are not seeing fair performance in how we are paid for the care we provide — and if denials and delays are not within a reasonable sphere of performance — then we are not going to continue working with that commercial payer,” Mr. Wexler said. “It’s time for us to reset the way the program works.”
Providence’s internal data highlights the pressure.
Compared to traditional Medicare, Medicare Advantage plans are 70% more likely to deny claims due to incomplete medical records and twice as likely to deny based on medical necessity, according to Mr. Wexler. Requests for additional documentation are 7.5 times higher, and the system has seen a 73% increase in payment denials and underpayments.
“Even before H.R. 1 came to life, the deterioration in commercial payer performance on Medicare Advantage was substantial,” he said.
Providence leaders argue that this level of friction diverts resources from patient care and imposes hundreds of millions of dollars in administrative burden. Mr. Wexler has called for stronger federal oversight, including support for the Medicare Advantage Prompt Pay Act, which would require MA plans to pay most clean claims within defined timeframes.
Mayo Clinic’s selective strategy
Rochester, Minn.-based Mayo Clinic has also adopted a more selective approach. In January, it ended contracts with most Humana and UnitedHealthcare Medicare Advantage plans.
“There’s been a significant amount of peer and network disruption in the Medicare Advantage space, and Mayo Clinic is taking a fairly aggressive approach,” CFO Dennis Dahlen said Nov. 5 during a fireside chat at Becker’s CEO+CFO Roundtable.
Mayo’s strategy is not an outright rejection of Medicare Advantage, but a recalibration.
“We’re being very selective about which Medicare Advantage plans we contract with,” Mr. Dahlen said. “But for those that we’re not in network with, patients likely won’t be able to get an appointment unless it’s clinically significant or we can make an exception.”
For every network decision, Mayo has built in clinical safety nets to preserve continuity for patients undergoing active treatment. But Mr. Dahlen warned that the current trajectory — marked by annual network disruptions and contract terminations — is unsustainable.
“Seniorhood is when we need healthcare the most,” he said. “That should be the last point in life where you’re at risk of losing network access.”
Ascension taking a closer look at Medicare Advantage
St. Louis-based Ascension, a 90-hospital system, is also scrutinizing Medicare Advantage more closely.
Eduardo Conrado, president and CEO, believes the program has drifted far from its original purpose.
“Congress created Medicare Advantage to deliver better benefits, broader coverage and lower costs for seniors,” Mr. Conrado told Becker’s. “Too often, that is not what patients experience.”
Like Providence, Ascension’s data show Medicare Advantage plans are 70% more likely than traditional Medicare to deny claims due to incomplete medical records and twice as likely to deny based on medical necessity. Most denials are eventually overturned, but only after time-consuming appeals.
“That process creates unnecessary stress for patients and delays in care,” Mr. Conrado said. “It also pulls doctors and nurses away from patient care and into administrative back and forth with insurers.”
Ascension has gone out of network in certain markets before returning to the table under revised terms. For example, Ascension Wisconsin recently went out of network with UnitedHealthcare before reaching a new deal in October
As contracts come up for renewal, Mr. Conrado said the health system is prepared to hold firm on expectations around timely payment, reduced administrative burden and patient access.
“We will focus on payers willing to work with us to support sustainable care for Ascension’s patients enrolled in Medicare Advantage plans,” he said.
What Medicare Advantage breakups mean for patient care
As more systems exit or narrow participation in the program, the implications for patients are becoming more visible.
For relatively healthy seniors, Medicare Advantage can offer lower premiums and additional benefits. But when patients develop complex or high-acuity conditions, narrow networks and prior authorization requirements can become barriers.
When Scripps exited Medicare Advantage, some patients expressed frustration. Others switched coverage to maintain access.
However, moving back to traditional Medicare is not always simple.
Barry Arbuckle, PhD, president and CEO of Fountain Valley, Calif.-based MemorialCare Health System, told Becker’s seniors who attempt to buy Medigap coverage after leaving Medicare Advantage may face medical underwriting, higher premiums or denial altogether — particularly if they have multiple chronic conditions.
For providers, the risk is that escalating contract disputes create instability at the very moment seniors need predictable access to care.
“If the end of the food chain isn’t compensated appropriately, providers will either close or exit those contracts — and the cycle will start all over again,” Mr. Van Gorder said.
That cycle could leave patients caught between network disruptions and rising out-of-pocket costs.
A tipping point?
Medicare Advantage is unlikely to disappear. Enrollment continues to grow — though at a slower rate — and bipartisan political support remains strong.
But the economics for providers are under strain.
Hospitals are facing what Providence leaders have dubbed a “polycrisis“: rising labor costs, inflation in supplies and equipment, looming Medicaid cuts and reimbursement pressures from traditional Medicare and commercial payers.
In that context, absorbing consistent Medicare Advantage losses becomes harder to justify, no matter how much infrastructure has already been built.
“The misguided belief among health systems is that you can make money providing Medicare Advantage as insurance,” Mr. Tande said, adding that neither the data nor Scripps’ experience supports that conclusion.
For many systems, the question is no longer whether Medicare Advantage is philosophically aligned with value-based care. It is whether the financial model — as currently structured — works.
If it does not, more providers may confront the same “sunk-cost” dilemma Scripps faced in 2024: stay in a system that erodes margins, or take the short-term pain of exit in pursuit of long-term stability.
As Mr. Dahlen put it, the current trajectory is unsustainable.
“While I don’t know exactly how this will play out, the current path — where there’s massive annual disruption around network participation, plan exits and coverage drivers — is one that can continue,” he said.
Whether through federal reform, payer recalibration or providers stepping back, something will have to give.
The post Medicare Advantage’s ‘sunk-cost’ problem appeared first on Becker’s Hospital Review | Healthcare News & Analysis.
Trump administration eyes US-run WHO alternative: Washington Post
After exiting the World Health Organization in January, the Trump administration is proposing to spend $2 billion annually on a U.S.-run replacement, The Washington Post reported Feb. 19.
The effort would replicate systems provided by the WHO, including laboratories, rapid-response systems and data-sharing networks, three administration officials briefed on the proposal told the Post.
“HHS is working with the White House in a deliberative, interagency process on the path forward for global health and foreign assistance that first and foremost protects Americans,” HHS spokesperson Andrew Nixon said in a statement shared with Becker’s on Feb. 19. HHS did not confirm the proposal.
President Donald Trump signed an executive order in January 2025 to withdraw the U.S. from the WHO effective Jan. 22, 2026, citing the global agency’s “mishandling of the COVID-19 pandemic” and other global health crises. However, the administration has not met one exit requirement: paying outstanding dues. The U.S. does not plan to pay the $278 million it owes for the 2024-25 period, NPR reported Jan. 20.
The alternative under consideration would cost about three times what the U.S. paid to the WHO annually, according to the Post.
“This $2 billion in funding to HHS is to build the systems and capacities to do what the WHO did for us,” one official told the newspaper.
Public health experts said the replacement likely would not match the WHO’s reach. The global agency provides access not offered to the U.S., such as to China and Russia, which do not typically share health information directly with the U.S., Atul Gawande, MD, the assistant administrator for global health for the U.S. Agency for International Development from 2022 to 2025, told the Post.
The post Trump administration eyes US-run WHO alternative: Washington Post appeared first on Becker’s Hospital Review | Healthcare News & Analysis.
AHA recommends ‘zero trust’ for cybersecurity
The American Hospital Association is suggesting that hospitals and health systems consider deploying “zero trust” architecture to improve their cybersecurity.
The National Security Agency recently released implementation guidelines for zero trust, a strategy that assumes no users or devices are safe and they must always be verified, according to a Feb. 19 AHA news release. The strategy, however, is expensive and may be cost-prohibitive to some organizations.
“With cybersecurity threats and attacks continuing to target the healthcare sector, adopting zero trust can help hospitals and health systems further reduce their cyber risk through a structured process,” stated Scott Gee, AHA deputy national advisor for cybersecurity and risk. “The NSA guidance is very detailed, and, while not tailored to healthcare, the process can be adapted to meet the needs of hospitals and health systems.”
The post AHA recommends ‘zero trust’ for cybersecurity appeared first on Becker’s Hospital Review | Healthcare News & Analysis.
Sanford Health regional CEO takes helm
Jason Caron, MD, has stepped into his role as president and CEO of Sanford Health in Bemidji (Minn.).
“After more than 20 years in this hospital, one thing remains clear: rural health care works best when the community and the hospital support each other,” he wrote in a Feb. 13 LinkedIn post.
Dr. Caron joined Sanford Bemidji Medical Center as a physician in 2004 and became CEO in January, according to his LinkedIn profile.
He succeeded Karla Eischens, who retired at the end of 2025 after 21 years with Sioux Falls, S.D.-based Sanford Health, including serving as CEO since 2022, according to a July 28 health system news release. Under her leadership, Sanford Bemidji expanded access to behavioral health with the region’s first crisis center and expanded its heart and vascular center.
The post Sanford Health regional CEO takes helm appeared first on Becker’s Hospital Review | Healthcare News & Analysis.
NYC Health + Hospitals unveils $2M MRI suite
New York City-based NYC Health + Hospitals/Jacobi | North Central Bronx unveiled a new $2 million MRI suite at its North Central Bronx campus.
The upgrade includes renovated rooms and new MRI machines, which the system said offer faster scan times and clearer, more distinct images to improve diagnostic capabilities and reduce patient wait times, according to a Feb. 19 news release. The machines also feature video projection to provide a calming virtual experience and technology designed to reduce scanner noise.
Leaders said in the release that the new MRI system is part of the hospital’s effort to enhance imaging services and improve productivity and imaging quality.
The post NYC Health + Hospitals unveils $2M MRI suite appeared first on Becker’s Hospital Review | Healthcare News & Analysis.
Walgreens to cut 628 jobs
Walgreens is laying off hundreds of employees in two states as its new private equity owner looks to cut costs, Bloomberg reported Feb. 19.
The company is eliminating 469 jobs in Illinois, where it is based, and plans to cut another 159 positions in Texas, where it is closing a distribution center. The figures were disclosed in letters sent to the states earlier in February, the report said.
Walgreens was acquired in August by Sycamore Partners after years of declining profitability. In a letter to the Illinois Department of Commerce and Economic Opportunity, a Walgreens representative said the company is reorganizing areas of the business “to best position the company for growth and deliver results where they matter most: in our stores and with our customers and patients.”
The post Walgreens to cut 628 jobs appeared first on Becker’s Hospital Review | Healthcare News & Analysis.
Top 10 hospitals for cost efficiency: Lown Institute
The Lown Institute Hospitals Index named the top 10 hospitals for cost efficiency.
The institute used clinical outcomes and cost Medicare fee-for-service claims for patients hospitalized from 2020 to 2022. The cost efficiency metric includes sub-metrics for 30- and 90-day cost efficiency, and measures risk-standardized hospital mortality rates against cost of care for Medicare patients. Hospitals with the lowest mortality and costs received the best scores in cost efficiency. Patients who were transferred, had COVID-19 or whose primary payer was not Medicare were excluded. Read the full methodology here.
The average mortality rate for all acute care hospitals was 9.5% and the average payment amount was about $17,500, according to a Feb. 19 institute news release.
The top 10 acute care hospitals had average risk-adjusted 30-day mortality rates under 7% and payments under $16,000. The lowest average mortality rate was 4.88%, and the lowest average payment was $11,366; these measures were not from the same hospital.
Here are the top 10 acute hospitals for cost efficiency.
- Davie Medical Center (Bermuda Run, N.C.)
- Northwestern Medicine Lake Forest (Ill.) Hospital
- Brigham and Women’s Faulkner Hospital (Boston)
- Northwestern Memorial Hospital (Chicago)
- Kuakini Medical Center (Honolulu)
- Barnes-Jewish West County Hospital (Creve Coeur, Mo.)
- UC Health Highlands Ranch (Colo.) Hospital
- Houston Methodist Hospital
- MultiCare Covington (Wash.) Medical Center
- Alta View Hospital (Sandy, Utah)
The post Top 10 hospitals for cost efficiency: Lown Institute appeared first on Becker’s Hospital Review | Healthcare News & Analysis.
CEO tapped to lead 3 New York City hospitals post-merger
NYC Health + Hospitals has appointed Svetlana Lipyanskaya as the next CEO of Maimonides Health, pending formal approval of the partnership between the two New York City-based health systems.
Ms. Lipyanskaya has served as CEO of NYC Health + Hospitals/South Brooklyn Health since 2020 and is part of the leadership team overseeing the integration of the two systems, according to a Feb. 19 NYC Health + Hospitals news release.
Manjinder Kaur, DNP, RN, would become CEO at South Brooklyn Health. She has served as the hospital’s COO since June 2024 and has been with NYC Health + Hospitals since 2006.
Maimonides Health and NYC Health + Hospitals are finalizing terms of a partnership supported by $2.2 billion over five years from New York state to protect safety-net healthcare in Brooklyn. Under the partnership, Maimonides would bring its three hospitals and more than 80 care sites under the public health system.
Ken Gibbs has served as president and CEO of Maimonides Health since 2022 and previously led Maimonides Medical Center since 2016. He has collaborated with Ms. Lipyanskaya on the partnership and leadership transition, he said in the release.
“It is a privilege to welcome Svetlana to the Maimonides family,” Mr. Gibbs said. “… I have known her for years and, most recently, we have been working together to bring Maimonides into NYC Health + Hospitals and lay the foundation for a successful transition and launch to further serve our communities and support the outstanding Maimonides team.”
During her tenure at South Brooklyn Health, Ms. Lipyanskaya oversaw the opening of a $923 million inpatient care facility in 2023 and led efforts that improved South Brooklyn Health’s The Leapfrog Group grade from a “D” to a “B.”
NYC Health + Hospitals operates 11 hospitals and employs more than 46,000 people.
The post CEO tapped to lead 3 New York City hospitals post-merger appeared first on Becker’s Hospital Review | Healthcare News & Analysis.
Seton Medical Center nurses call off strike after tentative agreement
Members of the California Nurses Association have called off their one-day strike planned for Feb. 19 after reaching a tentative labor contract with AHMC Seton Medical Center in Daly City, Calif.
The union — which represents about 300 nurses at the hospital, according to a Feb. 18 CNA news release — said the agreement addresses the issues nurses were set to strike over, namely safe staffing, and recruitment and retention.
“The nurses made it clear what needs to be done in order for us to provide optimal care for our patients and our community,” Michelle Kubota, RN, said in the release. “We are encouraged that our solidarity resulted in a tentative agreement. We will now put this tentative agreement to a vote.”
Becker’s has reached out to Seton and will update this story if a comment is received.
Contract talks began in January 2025. Nurses voted to authorize a strike in December.
The post Seton Medical Center nurses call off strike after tentative agreement appeared first on Becker’s Hospital Review | Healthcare News & Analysis.
CommonSpirit California CFO transitions to new regional role
Shelly Schorer, California CFO at Chicago-based CommonSpirit Health, has accepted a role as the system’s South region CFO, effective March 1, according to a Feb. 19 LinkedIn post.
CommonSpirit South Region comprises 42 acute care, specialty and critical access hospitals and spans across Arkansas, Kentucky, Ohio, Tennessee, North Georgia and Texas. It has ambulatory surgery centers, imaging centers urgent care sites and cancer centers with more than 31,000 employees, Ms. Schorer said in the post.
“My time in California for the last 9 years has been so wonderful and I have grown and learned so many things and had so many wonderful experiences and built a great team,” She said. “I am excited for the new challenges ahead and will miss my colleagues and friends in California.”
The post CommonSpirit California CFO transitions to new regional role appeared first on Becker’s Hospital Review | Healthcare News & Analysis.
Nearly 90% of healthcare organizations say modernization is essential: Survey
Nearly 90% of healthcare organizations say they must modernize operations to keep pace with mounting clinical, regulatory and financial pressures, according to a new survey of healthcare technology leaders.
The 2026 Leadership Pulse Survey from the College of Healthcare Information Management Executives, conducted by RLDatix, found broad concern that fragmented technology systems and disconnected data environments are hindering organizational performance and, in some cases, creating patient safety risks.
Here are six key findings from the survey:
- Respondents signaled that modernization is no longer optional. Nearly 90% said their operations must evolve to address rising complexity, and 80% identified interoperability as a baseline expectation for coordinated execution.
- The survey also highlighted operational strain caused by what many leaders describe as tool sprawl. Seventy-six percent of respondents reported that managing too many point solutions makes operations more difficult. Some organizations said they operate more than 100 tools across the enterprise, including 10 to 20 systems dedicated to safety, compliance, provider management and patient experience.
- More than three-quarters of respondents said working across multiple tools is central to their challenges. When issues stall during handoffs between systems and teams, they remain unresolved longer, increasing risk across safety, compliance, provider management and patient experience functions.
- Interoperability is increasingly shaping technology decisions. Eighty percent of respondents said it is a top priority, and 74% said integration with existing systems, including the electronic health record, is a key factor in selecting future platforms. Leaders also are evaluating whether data can remain standardized and accessible during system transitions or downtime.
- Financial pressures are influencing modernization strategies as well. Eighty-five percent of respondents cited budget constraints as the leading barrier to change. At the same time, 70% said reducing total cost of ownership is a key consideration in platform selection, and 31% said they are actively exploring vendor consolidation.
- Rather than adding more systems, leaders are focusing on simplifying their environments by reducing coordination burden, retiring legacy platforms without losing historical records and strengthening accountability across workflows.
The post Nearly 90% of healthcare organizations say modernization is essential: Survey appeared first on Becker’s Hospital Review | Healthcare News & Analysis.
Scripps Health posts 4.1% operating margin in Q1
San Diego-based Scripps Health recorded an operating income of $52.2 million (4.1% operating margin) in the first quarter of fiscal 2026, down from an operating income of $67.3 million (5.5% margin) during the same period last year.
Scripps reported total operating revenue of $1.3 billion for the three months ended Dec. 31, up from $1.2 billion during the same period last year. Patient service revenue was $1.1 billion, up from $1 billion. Scripps did not record California Provider Fee income in the first quarter due to the delay in program approval for calendar years 2025 and 2026. The system reported $42.8 million in provider fee revenue during the first quarter last year.
Total operating expenses were $1.22 billion, up from $1.16 billion during the same quarter last year. Wages and benefits totaled $522.5 million, up from $492.5 million, primarily driven by staffing increases. Supply expenses were $244.1 million, up from $215.1 million. Scripps did not record a provider fee expense in the first quarter of 2026 due to the delay in program approval, but recorded an expense of $35.9 million during the first quarter last year.
Scripps had 420 days cash on hand as of Dec. 31, up from 418 on Sept. 30.
The system reported a net income of $118.3 million in the first quarter of 2026, up from $4.8 million last year.
The post Scripps Health posts 4.1% operating margin in Q1 appeared first on Becker’s Hospital Review | Healthcare News & Analysis.
McLaren hospital taps chief nurse
McLaren Central Michigan in Mount Pleasant has named Kelly DeBolt, BSN, RN, chief nursing officer.
Ms. DeBolt will lead a team of more than 100 nurses at the hospital, according to a news release shared with Becker’s Feb. 19. She joins Grand Blanc, Mich.-based McLaren Health Care from Select Specialty Hospital in Saginaw, Mich., where she spent the past four years as CEO.
Ms. DeBolt’s career in healthcare began more than 20 years ago as a bedside nurse. She has since served in leadership roles ranging from clinical support to risk management and operations.
The post McLaren hospital taps chief nurse appeared first on Becker’s Hospital Review | Healthcare News & Analysis.
UChicago Medicine names Medical Center president
Krista Curell, RN, was appointed president of the University of Chicago Medical Center, effective late 2025.
Ms. Curell will continue serving in her prior roles as president of UChicago Medicine Crown Point (Ind.) and executive vice president and system COO at UChicago Medicine, according to a Feb. 19 health system news release.
In her new role, she will also lead day-to-day operations and strategy for the academic medical center and oversee more than 14,000 employees and 2,400 clinicians across the health system’s hospitals, clinics and physician practices in Chicago, its suburbs and Northwest Indiana. She will continue reporting to Tom Jackiewicz, president of UChicago Medicine, who previously held the Medical Center president title in addition to leading the health system.
Ms. Curell also oversees several major initiatives, including a 575,000-square-foot cancer pavilion slated to open in 2027, a forthcoming clinical laboratory and education center in Washington Park in partnership with City Colleges of Chicago, and UChicago Medicine Crown Point, the release said.
She was appointed executive vice president and system COO in 2023. Before that, she served as executive vice president and chief integration and transformation officer beginning in March 2021.
The post UChicago Medicine names Medical Center president appeared first on Becker’s Hospital Review | Healthcare News & Analysis.
Payer, provider transparency campaigns could signal deeper tensions
Recently, payers and providers have been engaging in a slew of transparency campaigns, with some aiming to “expose” pricing and denial concerns.
For example, Hospital Watch has come to the forefront, shifting blame to hospitals.
“Hospital Watch is a watchdog group dedicated to shining a light on corporate hospitals as the top culprit in driving up U.S. healthcare costs — exposing corporate hospitals’ monopolistic practices in price gouging patients with excessive markups and hidden fees with no transparency while forcing patients and employers to pay more for their care,” the group’s website says.
While Hospital Watch said its focus is corporate hospitals, a map showing payment incidents across the U.S. also features nonprofits and academic medical centers. Better Solutions for Healthcare — which includes the BCBS Association and AHIP as members — oversees the project, and former congressional staffer Adam Buckalew advises.
BCBS Vermont was behind the Vermont Affordable Care campaign, consisting of a website and local ads. The initiative focuses on comparing pricing at academic medical centers and independent facilities. A spokesperson for BCBS of Vermont previously said the effort aims “to educate.”
Insurers are not the only ones launching such campaigns. The Indiana Hospital Association’s Access Denied initiative focuses on care denials and intends “to expose abusive insurer practices.” IHA President Scott Tittle advocated for legislative reform, pointing to a state bill that would prevent imposing penalties on facilities using out-of-network providers, as well as another that would restrict downcoding, block retroactive payment rate reductions and limit clawbacks.
Despite IHA’s efforts, Elevance Health — one of the campaign’s main targets — said it is engaging in “collaborative work with providers” to lower costs.
In an interview with Becker’s, BCBS Vermont President and CEO Beth Roberts said she admires her team’s consumer awareness work, which predates her appointment. While Lebanon, N.H.-based Dartmouth Health told Becker’s it did not know about the campaign at the time, Ms. Roberts said she has been in affordability talks with University of Vermont Health CEO Stephen Leffler, MD. The campaign claimed UVM Medical Center was the most expensive listed facility as of Oct. 1, followed by Dartmouth Health.
Becker’s contacted Mr. Buckalew’s strategic advisory firm, ALB Solutions, and will update this story if more information becomes available.
The post Payer, provider transparency campaigns could signal deeper tensions appeared first on Becker’s Hospital Review | Healthcare News & Analysis.
Trinity Health hospital nurses ratify 3-year labor deal
Nurses at St. Mary Medical Center in Langhorne, Pa., have ratified a three-year labor contract, according to a Feb. 18 news release from the Pennsylvania Association of Staff Nurses and Allied Professionals, which represents the workers.
The agreement covers 630 registered nurses at the 373-bed hospital. Union officials said 94% of participating nurses voted in favor of ratification.
Under the contract, staffing grids are locked in through Dec. 31, 2027, with no changes permitted, according to PASNAP. The agreement also includes base wage increases of up to 17% over three years and higher shift differentials for evening, night, weekend and pool nurses.
“Highly skilled, experienced nurses are the backbone of healthcare, bringing to the bedside well-honed intuition, leadership and institutional knowledge,” Debbi Bozeman, RN, a nine-year St. Mary nurse, said in the release. “We need seasoned nurses; our patients need seasoned nurses. And this contract respects the expertise seasoned nurses bring to the bedside and rewards the essential role we play in patient care.”
The hospital is part of Trinity Health Mid-Atlantic, based in Newtown Square, Pa., a regional division of Livonia, Mich.-based Trinity Health.
In a statement shared with Becker’s, St. Mary said, “[T]he contract, which includes competitive wages and continued investment in a positive working environment, reflects our shared commitment to delivering high-quality, compassionate care to the patients and communities we serve.
“We are proud to reach an agreement that is in the best interest of our colleagues and patients — with a focus on supporting our nurses in their essential role — while helping to ensure that St. Mary continues to deliver exceptional patient care in support of our mission to serve as a compassionate and transforming healing presence within our communities.”
The post Trinity Health hospital nurses ratify 3-year labor deal appeared first on Becker’s Hospital Review | Healthcare News & Analysis.
How Care New England is embedding Epic training into nursing education
Providence, R.I.-based Care New England has partnered with Rhode Island College in Providence to create a pipeline of digitally educated, EHR-trained nurses and healthcare administrators, Tomas Gregorio, CIO of the health system, told Becker’s.
The partnership, announced Feb. 5, aims to build a pipeline of nurses and healthcare technology professionals trained in cybersecurity, AI, data analytics and digital health. Under the partnership, Care New England will work with the college to enhance existing academic programs and develop new clinical and healthcare management degree programs, professional certifications and workshops.
“It will allow us, as we start to recruit and grow Care New England, to build a certified and trained group of individuals who come in with education on how Care New England works — how a hospital works, how administration looks at dashboards to make critical operational decisions,” he said.
As health systems continue to face significant nursing shortages, Mr. Gregorio said organizations should build closer relationships with nursing schools. However, this partnership goes further. A key element of the collaboration includes integrating Epic EHR training into Rhode Island College’s nursing and health sciences curricula.
Care New England will provide access to an Epic academic license, allowing students to gain hands-on experience with the EHR platform. The partnership also includes the creation of internship and cooperative education opportunities for Rhode Island College students, which could lead to full-time employment with Care New England.
“We want those nurses to have an idea of what the EHR looks like before they join us,” Mr. Gregorio said.
He added that the Epic experience will help students enter internships or co-ops with an understanding of real software dashboards that show what running a hospital or hospital department looks like, expediting onboarding for Care New England and other organizations that may hire them.
“Getting talent early, teaching them how Epic works and ensuring that when they become part of your organization they already understand how to do the work — that’s extremely important,” he said. “Through internships and co-ops, you can test individuals, see how they function in the environment and make better hiring decisions.”
As for the end goal, Mr. Gregorio said he hopes the partnership strengthens Rhode Island’s health IT presence.
“That’s the bigger goal. Rhode Island College specializes in workforce development, and we believe this partnership creates a strong transition from education into the workforce,” he said. “They need to educate students, and we need to hire them — especially as we continue growing the workforce.”
The post How Care New England is embedding Epic training into nursing education appeared first on Becker’s Hospital Review | Healthcare News & Analysis.
2 Connecticut cities accuse PBMs, drugmakers of ‘insulin pricing scheme’
Two Connecticut cities filed federal lawsuits against Cigna, CVS Health and UnitedHealth Group — targeting their pharmacy benefit managers — over an alleged “insulin pricing scheme,” according to January filings in the U.S. District Court for the state.
Along with Express Scripts, Evernorth, CVS Caremark and Optum Rx, Norwalk and New Haven’s lawsuits focus on drug manufacturers Eli Lilly and Co., Novo Nordisk and Sanofi, as well as group purchasing organizations.
The cities characterize themselves as operators of self-funded plans and said they were “significantly overcharged” for insulin. The complaints accuse parties of fraudulent activity and violations of federal anti-racketeering laws, and state and federal antitrust laws. Norwalk and New Haven are seeking monetary damages, restitution, attorney fees and injunctions to halt this conduct.
“Pharmaceutical companies alone are responsible for the prices they set in the marketplace for the products they manufacture. Nothing in our agreements prevents drug manufacturers from lowering the prices of their insulin products, and we would welcome such an action,” a CVS Caremark spokesperson said in a statement shared with Becker’s. “Allegations that we play any role in determining the prices charged by manufacturers for their products are false, and we intend to vigorously defend against this baseless suit.”
A statement from Optum Rx echoed this, adding the PBM “has aggressively and successfully negotiated with drug manufacturers and taken additional actions to lower prescription insulin costs for our health plan customers and their members.”
“PBMs, like Optum Rx, are the key counterweight to pharmaceutical companies’ otherwise unchecked monopoly power to set and raise drug prices,” the company said.
Novo Nordisk, however, also called the allegations “meritless.”
“We intend to vigorously defend against these claims,” a spokesperson said in a statement. “While we will not comment further about pending litigation, we recognize that not all patient situations are the same and we have a number of different insulin affordability offerings available through NovoCare. Importantly, we continually review and revise our offerings as well as work with diverse stakeholders to create solutions for differing patient needs.”
The lawsuits were filed shortly before the Federal Trade Commission reached a settlement with Cigna’s Express Scripts, aiming to lower out-of-pocket costs for drugs like insulin by $7 billion over a decade. The Labor Department had also pushed for greater transparency between PBMs and self-insured group health plans through proposed regulation.
Becker’s contacted Cigna, Eli Lilly and Sanofi and will update this story if more information becomes available.
The post 2 Connecticut cities accuse PBMs, drugmakers of ‘insulin pricing scheme’ appeared first on Becker’s Hospital Review | Healthcare News & Analysis.
How CHS sold 35% of its hospitals and held revenue
Franklin, Tenn.-based Community Health Systems has divested around 35% of its portfolio since 2019, but net revenue has stayed relatively the same, shifting slightly from approximately $13 billion in 2019 to $12.5 billion in 2025.
“The EBITDA is also relatively close, even though we have 35% fewer facilities,” Kevin Hammons, CEO of CHS, said in a Feb. 19 earnings call.
CHS reported an operating income of $450 million (14.5% margin) in the fourth quarter ended Dec. 31, 2025, up from a $279 million (8.5% margin) in the same quarter last year. Total revenue for CHS was $3.1 billion in the fourth quarter, down from $3.3 billion over the prior-year period and total expenses were $2.7 billion, down from $3 billion in the same quarter last year.
CHS completed seven hospital divestitures in 2025, with deals closing at regular intervals throughout the year. Three involved partial ownership sales, including 50% stakes in two facilities and an 80% stake in a third, while four others were sold outright. It also sold certain ambulatory outreach laboratory assets in December to LabCorp for $194 million and received an additional $91 million in October related to its August 2024 divestiture of Tennova Healthcare-Cleveland.
The health system then sold three Pennsylvania hospitals to Tenor Health Foundation for $33 million in cash, including a $15 million promissory note, which closed Feb. 1, 2026. It also off-loaded Tennova Healthcare-Clarksville (Tenn.) to Nashville, Tenn.-based Vanderbilt University Medical Center on Feb. 1, 2026, for $623 million and signed a $450 million deal in January 2026 to sell Crestwood Medical Center in Huntsville, Ala., to Huntsville Hospital Health System.
“As we divest facilities and reduce the number of transactions we’re processing, we can scale those accordingly,” Mr. Hammons said. “Keep in mind, we’ve been adding significant numbers of beds to our existing hospitals, even though we’ve been divesting some hospitals with our capital projects over the last several years.”
Mr. Hammons said CHS has added 500 to 600 beds to its core portfolio over the last three to four years, including freestanding emergency departments, surgery centers and clinics.
The operational moves appear to be paying off on the system’s balance sheet. Jason Johnson, executive vice president and CFO of CHS, said during the call that the health system’s net debt has also fallen from $11.4 billion at the end of 2024 to a projected $9.2 billion once the Alabama sale closes, a more than $2 billion reduction in just over a year.
Following its divestitures, CHS has not completely ruled out other sales.
“We still have some inbound interest as we continue, and probably will always have some inbound interest because we have some very good markets,” Mr. Johnson said. “There are a couple transactions right now that we are in some early stages of discussions, but we are not sure yet whether those will proceed or whether we will be able to get those across the finish line. I would say, in terms of what we have, the interest in selling is certainly dwindling.”
The post How CHS sold 35% of its hospitals and held revenue appeared first on Becker’s Hospital Review | Healthcare News & Analysis.
HCA Alaska Hospital taps 4 new leaders
Nashville, Tenn.-based HCA Healthcare’s Alaska Regional Hospital in Anchorage has named four new leaders.
The appointments come less than a year after the hospital named five new C-suite leaders, including a new CEO.
Melissa Butler was named COO, according to a Feb. 5 hospital statement shared with Becker’s. She brings more than 20 years of healthcare experience, including nine years with HCA Healthcare. She previously held leadership roles within the system’s Gulf Coast Division and at Corpus Christi (Texas) Medical Center.
Yvonne Schofield was appointed vice president of operations. She brings more than 20 years of nursing and healthcare leadership experience to the role and most recently served as director of surgical services at Corpus Christi Medical Center.
Mike Davis, MSN, was named vice president of quality. He joined the hospital four years ago as a clinical quality coordinator and was later named stroke program coordinator.
Montana Miller was appointed vice president of human resources. She previously led human resources at Anchorage-based North Star Behavioral Health and has experience in healthcare and other industries.
The post HCA Alaska Hospital taps 4 new leaders appeared first on Becker’s Hospital Review | Healthcare News & Analysis.
Optum launches latest AI tool to support value-based care
Optum has launched Value Connect, an AI-powered platform designed to help payers and providers operationalize value-based care models by combining clinical, operational and financial data into a single system.
The platform uses AI across quality measures, utilization patterns and risk indicators to flag patients who need intervention and route next steps directly into care team workflows. It is powered by more than 1,600 models, including Optum’s generative AI capabilities, and is designed to replace manual processes like spreadsheets and handoffs by embedding actionable steps into existing workflows, according to a Feb. 18 news release.
Optum said customers using Value Connect are seeing a 35% reduction in medical spending, 17% reduction in pharmacy costs, 29% fewer emergency room visits, 28% fewer preventable hospital readmissions and more than 20% improvement in care gap closure. The company did not specify how many customers the figures are based on or against what baseline the reductions were calculated.
The new platform is the latest in a series of AI-enabled products from Optum. Recent launches include prior authorization tools, a real-time claims validation platform, and a predictive analytics tool for operating room scheduling.
The post Optum launches latest AI tool to support value-based care appeared first on Becker’s Hospital Review | Healthcare News & Analysis.
The Value of Nurses on Boards Is No Longer Debatable
Michael Porter defined value as outcomes divided by cost1. Healthcare embraced the equation quickly but applied it unevenly. For decades, nurses have been treated primarily as a cost to be managed rather than as the people and capability that make outcomes possible. They are bundled into room charges, excluded from RVUs, and discussed more often as labor expense than as strategic assets. Yet nurses remain the largest segment of the healthcare workforce and the primary drivers of inpatient care, safety, and patient experience.2
For years, nurse leaders have asked how to assign value to nursing. The more urgent question today is simpler and more uncomfortable: how can healthcare be governed without nurses at the table?
Boards exist to steward trust, oversee risk, and ensure long-term viability. That responsibility becomes compromised when boards govern abstractions rather than the work itself. A healthcare board without nursing expertise is not balanced; it is incomplete. Most hospital and state healthcare association boards currently lack nurses as voting members of the board. Even when Chief Nursing Officers (CNOs) and Registered Nurse (RN) executives are present, formal governance power remains concentrated among Chief Executive Officers (CEOs) and other executive leaders. Representation without governing and voting authority creates an uneven table. The 2025 National Governance Report by the American Hospital Association states that the actual number of clinicians on hospital boards has decreased from 29% in 2014 to 26% in 2024. Physicians still make up most clinicians on hospital boards, but their proportion fell from 20% in 2014 to 16% in 2024. Nurses make up only 5% of clinicians on hospital boards and this is unchanged from 2014.3 This is not about representation. It is about whether governance reflects how care is actually delivered.
The breakdown becomes most visible around measurement. Leadership often says it wants better data on nursing. Nurses often resist being measured. The reason is not technical or ideological. It is trust. Trust that is visible and mutual.
Historically, healthcare made nurses’ work harder while removing the supports that once made the job doable. Unit clerks disappeared. Transport and ancillary roles thinned. Tasks that were never designed as nursing work were pushed onto nurses simply because someone had to absorb them. At the same time, patient acuity increased, technology proliferated, and documentation demands expanded relentlessly. Time-motion and EHR studies consistently show that nurses now spend roughly a third of their shift documenting care.4 That time does not replace patient care; it stacks on top of it.
This accumulation created a job that is no longer realistically finishable. The pandemic did not cause this. It exposed it.
In that context, resistance to measurement is rational. When visibility has historically preceded cuts rather than improvement, measurement feels like threat, not learning. The dominance of staffing ratios reflects this reality. Ratios are not what nurses want. They are the only measure nurses trust. They are blunt, incomplete, and insufficient—but they are defensible in a low-trust system. Ratios are not a solution; they are a symptom.
This is not a nursing failure or a leadership failure. It is a relationship failure, and therefore a governance failure. Measurement without trust is experienced as control. Measurement with trust becomes learning. And healthcare will not get better data, better workflows, or better outcomes until trust is addressed first.
That is precisely why nurses on boards matter.
As a nurse with more than four decades of experience across clinical care, administration, academia, and industry, I have focused this chapter of my career on bringing the nursing lens into governance. When I joined the Board of Directors at Children’s Mercy in Kansas City, MO, I was the only nurse and one of only a small number of clinicians. The response from nursing leaders was immediate. They did not experience it as symbolic. They experienced it as practical. For the first time, they believed decisions affecting their work would be shaped by someone who understood the realities they lived every day.
From the board side, the shift was equally tangible. Discussions about quality, safety, experience, and workforce sustainability became more grounded. Metrics were interrogated differently. Risks surfaced earlier. Strategy became more executable because it was anchored in how care actually happens, rather than how it is assumed to happen.
From a CEO perspective, this is not optional. Governing healthcare without nursing expertise is no longer defensible. A nurse on the board makes one governance question unavoidable: who was part of this decision? That question matters because the tradeoffs facing healthcare today are real and consequential. When nurses are part of governance, decisions become rounder and more credible. Consequences are anticipated rather than explained after the fact. And because nurses trust nurses, decisions shaped with nursing input land differently inside the organization.
The evidence supports what experience makes obvious. Higher patient-to-nurse ratios are associated with increased mortality, higher failure-to-rescue rates, and greater nurse burnout.5 Stronger nursing work environments are associated with better patient outcomes and improved retention.6 Missed nursing care is consistently linked to adverse outcomes.7,8 If boards care about outcomes, they must govern the conditions under which those outcomes are produced. One of the key tenets of high reliability is deference to expertise. Highly reliable organizations value expertise over authority and governance must reflect this principle.9
The important point is this: this is fixable. The AHA postulates that fewer clinicians on hospital boards may be the result of the difficulty in recruitment of clinical expertise outside of their own organizations.3 However, a large number of clinicians and nurse leaders specifically are in academia, self-employment, industry, and retirement. Perhaps recruitment needs to expand to these areas. But the first step is not a new metric, a new dashboard, or another performance initiative. The first step is trust. Trust is what allows transparency. Transparency allows learning. Learning allows redesign. Without trust, every attempt to “measure nursing better” will be interpreted as preparation for further extraction.
Boards helped create the conditions that made nursing work undoable. Boards therefore have a responsibility to help redesign it. That work cannot be done without nurses as full participants in governance.
This is now the baseline for competent healthcare governance.
References
- Michael Porter and Elizabeth Olmsted Teisberg, Redefining Health Care (Massachusetts: Harvard University Press, 2006), 4.
- American Association of Colleges of Nursing. Nursing Workforce Fact Sheet. 2024.
- American Hospital Association (2025). 2025 National Governance Report
- Bakhoum N, et al. Time and motion analysis of nurses’ EHR use.
- Cho H, et al. Nurses’ documentation burden and workflow.
- Aiken LH et al. Hospital nurse staffing and patient mortality, burnout, and job dissatisfaction. NEJM.
- Lake ET et al. Nurse work environments and patient outcomes.
- Nantsupawat A, et al. Missed nursing care and adverse outcomes.
“High Reliability,” Agency for Healthcare Research and Quality, updated July 2016, https://psnet.ahrq.gov/primers/primer/31/high-reliability.
The post The Value of Nurses on Boards Is No Longer Debatable appeared first on Becker’s Hospital Review | Healthcare News & Analysis.
In a cooling strike climate, healthcare heated up
Healthcare remains a focal point for work stoppages, despite a broader national decline, as hospital and health system employees continue to cite pay and staffing concerns.
Union activity in 2026 has already seen notable labor actions, such as the largest nurses strike in New York City history and an open-ended walkout by 31,000 United Nurses Associations of California/Union of Health Care Professionals members at Kaiser Permanente facilities. In total, Becker’s has reported on nearly a dozen strikes since the beginning of 2026 and nearly 40 in 2025.
New data, released Feb. 18, from the Labor Action Tracker’s “Annual Report 2025,” published by Cornell University’s School of Industrial and Labor Relations and the University of Illinois’ School of Labor and Employment Relations, show a substantial increase in work stoppages in the healthcare and social assistance sector from 2024 to 2025. The tracker compiles publicly reported strikes and lockouts using verified media, database and social media sources.
The report found that, while overall U.S. work stoppages declined nearly 16% over the past year, healthcare and social assistance saw a 58.3% increase in work stoppages and a 151.9% increase in the number of workers involved during the same period — the largest increase of any industry.
The report also found that healthcare and social assistance work stoppages increased from 36 involving 46,369 workers in 2024 to 57 involving 116,826 workers in 2025. The industry accounted for 40.3% of all striking workers, ahead of public administration at 29.6%, and ranked first in strike days with 1,213,703 — nearly double manufacturing’s 684,773.
Across all industries, the top reasons for work stoppages were pay (195), followed by first-contract negotiations (70) and healthcare benefits (66).
Healthcare strikes in 2025 were largely driven by pay and staffing concerns, Johnnie Kallas, PhD, who launched the Labor Action Tracker in 2021 and is an assistant professor at the University of Illinois School of Labor and Employment Relations, told Becker’s. Of the 54 strikes that began in 2025, staffing was a major demand in 34 and pay in 32.
“This is also important because strikes declined broadly in 2025 but increased considerably in healthcare,” Dr. Kallas said. “The number of strikes increased by 58.3%, and the number of workers involved in healthcare strikes increased by 151.9% from 2024 to 2025.”
“Healthcare workers continue to face inflationary pressures and a lack of respect on the job, while hospitals face financial pressures tied to inadequate reimbursement rates from public and private payers,” he added.
Hospital executives have described that same dynamic as a delicate balancing act. Greg Till, chief people officer of Renton, Wash.-based Providence, told Becker’s in October that systems are trying to “thread the needle” between managing tighter budgets and addressing rising labor costs and workforce expectations.
“We want to ensure we offer market-competitive pay and benefits for our caregivers while preparing for the financial pressures ahead,” Mr. Till said.
Dr. Kallas said early evidence from 2026 suggests the trend may continue, pointing to 15,000 New York State Nurses Association nurses in New York City and 31,000 Kaiser Permanente healthcare workers along the West Coast who have walked off the job this year.
As of Feb. 18, nurses at Montefiore, Mount Sinai Hospital and Mount Sinai Morningside and West have ratified new three-year contracts covering about 10,500 nurses across those systems. Roughly 4,200 nurses at NewYork-Presbyterian remain on strike, and the Kaiser Permanente strike that began Jan. 26 remains ongoing.
Dr. Kallas noted another major distinction with the recent actions: several have been open-ended rather than of a fixed duration.
“Most healthcare strikes are of a fixed duration,” he said. “The fact that we’re seeing more open-ended strikes indicates that workers are ready to fight for strong contracts despite a more hostile political environment for organized labor.”
The post In a cooling strike climate, healthcare heated up appeared first on Becker’s Hospital Review | Healthcare News & Analysis.
More than 20 health systems launch specialty care coalition to expand rural access
A new national coalition of health systems and strategic partners has launched to address worsening shortages in access to medical specialists in rural areas and underserved urban communities across the United States.
The National Specialty Care Access Coalition — a collaboration of more than 20 major U.S. health systems — aims to advance multispecialty, technology-enabled specialty care models designed to scale nationally and move beyond isolated pilot programs, according to a Feb. 18 press release announcing the group’s formation.
The coalition is convened and chaired by Chethan Sathya, MD, vice president of strategic initiatives at Northwell Health in New Hyde Park, N.Y., and Raj Narula, MD, founder and CEO of Sevaro. The coalition’s founding health systems collectively deliver care across rural regions and high-need urban communities nationwide.
The group’s launch comes as policymakers and health systems face intensifying pressure to rethink how specialty care is delivered, particularly with the introduction of the Centers for Medicare & Medicaid Services’ Rural Health Transformation initiative and more than $50 billion in new federal and state investment, the press release said.
The coalition said it will focus initially on three priorities: standardizing multispecialty care pathways for rural hospitals and high-need urban health systems; producing a white paper with recommendations for CMS and state Medicaid agencies; and accelerating real-world implementation through shared learnings and pilots in high-impact specialties.
The press release said additional thought partners include former CMS leaders, the Children’s Hospital Association, state hospital associations and the Center for Telehealth and eHealth Law. Technology collaborators named in the release include T-Mobile, Sevaro Health and Samsung, though the coalition said participation does not imply endorsement of any single technology platform.
The National Specialty Care Access Coalition said it will begin formal work in early 2026 and plans to invite additional health systems to submit expressions of interest as it expands.
The post More than 20 health systems launch specialty care coalition to expand rural access appeared first on Becker’s Hospital Review | Healthcare News & Analysis.
Georgia hospital reports 2025 hacking incident
Swainsboro, Ga.-based Emanuel Medical Center is notifying patients of a May 2025 hacking incident.
On May 22, the hospital detected suspicious activity on its computer systems and took steps to secure its network and investigate, according to the Feb. 17 notice. Emanuel Medical learned that an unauthorized party gained access to its systems, which contained patients’ personal and protected health information, from May 21-24.
“Once we identified the potentially affected files, we promptly engaged a data-review firm to determine what information was contained in those files,” the hospital stated. “We recently received the results of that review, and we have been working since that time to compile contact information for notifying impacted individuals.”
The breached data may have included names, dates of birth, Social Security or driver’s license numbers, health insurance information, and medical records.
The post Georgia hospital reports 2025 hacking incident appeared first on Becker’s Hospital Review | Healthcare News & Analysis.
Wellstar names chief strategy and growth officer
Thomas Kruse was appointed executive vice president and chief strategy and growth officer of Marietta, Ga.-based Wellstar Health System, effective March 30, according to a health system news release shared with Becker’s.
In his new role, Mr. Kruse will lead enterprise-level strategy and transformation, evaluate market expansion and affiliation opportunities, and drive initiatives to support the system’s long-term growth, the release said.
Most recently, he served as an independent health industry advisor and consultant for regional health systems, community hospitals and nonprofit organizations.
Previously, he was senior vice president and chief strategy officer for the Northwest Region of Chicago-based CommonSpirit Health and Tacoma, Wash.-based Virginia Mason Franciscan Health, where he led long-range strategy and partnership efforts. Earlier in his career, he served as chief strategy officer for Edison, N.J.-based Hackensack Meridian Health.
Wellstar is an 11-hospital system with more than 34,000 employees.
The post Wellstar names chief strategy and growth officer appeared first on Becker’s Hospital Review | Healthcare News & Analysis.
What’s driving system investments in rehab care?
So far in 2026, about half a dozen U.S. hospitals and health systems have said they plan to expand rehabilitation services as organizations aim to ease capacity strains and meet rising demand.
In January, Springfield, Ill.-based Hospital Sisters Health System and Brentwood, Tenn.-based Lifepoint Health said they are partnering on a 40-bed inpatient rehabilitation hospital under construction in Howard, Wis. The freestanding facility will double inpatient rehabilitation capacity currently at HSHS St. Vincent Hospital in Green Bay, Wis., allowing the hospital to repurpose its existing rehab unit to support acute care demand.
A few weeks later, Birmingham, Ala.-based Encompass Health said it is planning a freestanding 50-bed inpatient rehabilitation hospital in Flowood, Miss., set to open in 2027. With 173 hospitals across 39 states and Puerto Rico, Encompass is the largest owner and operator of rehabilitation hospitals in the U.S.
Other health systems that have recently opened or announced plans to expand rehabilitation services include Jacksonville, Fla.-based Baptist Health, Birmingham, Ala.-based UAB Medicine, Oakland, Calif.-based Kaiser Permanente, Sarasota (Fla.) Memorial Health Care System and Winston-Salem, N.C.-based Novant Health.
Relieving hospital capacity pressure
Many of these projects are tied to broader operational challenges, as hospitals report elevated inpatient volumes and longer lengths of stay, driven in part by higher-acuity patients and limited post-acute capacity. Skilled nursing facilities in many markets remain constrained by workforce shortages, reducing discharge options for patients who no longer require acute care but need intensive therapy.
Expanding inpatient rehabilitation facilities allows systems to move appropriate patients out of acute beds more efficiently while keeping them within their networks. In some cases, as with HSHS St. Vincent Hospital, rehab expansion enables hospitals to convert space back to higher-demand acute services.
Growing clinical demand
Demand for rehabilitation services is also increasing.
Industry projections show the global rehabilitation market is expanding, driven by population aging and a growing number of patients with neurological, musculoskeletal and cardiologic conditions.
Additionally, advances in stroke, trauma and cardiac care mean more patients are surviving complex events but require intensive care from health systems.
A market-specific strategy
Not all hospital systems are expanding their rehabilitation footprint, though. Kaleida Health’s Buffalo (N.Y.) General Medical Center, for example, plans to reduce beds in its medical rehab unit from 34 to 16 as part of a broader $200 million strategic plan.
“The remaining 18 beds from the MRU will be repurposed to much-needed inpatient capacity,” Kaleida Health said in a statement. “Patients who require MRU-level care beyond the remaining 16 beds have access to several other MRUs within the community, ensuring continuity of care.”
The variation underscores that rehabilitation strategy depends on local market dynamics. In markets facing post-acute shortages and rising acuity, however, inpatient rehab is increasingly viewed as both a clinical necessity and an operational pressure valve.
The post What’s driving system investments in rehab care? appeared first on Becker’s Hospital Review | Healthcare News & Analysis.
Hospice spending, care quality scores by state
California and Nevada hospice providers had the lowest care-quality scores despite spending the most per beneficiary to provide care between Jan. 1, 2023, and Dec. 31, 2024, according to CMS data released Feb. 18.
Rhode Island and West Virginia had the highest hospice care quality scores during the data collection period.
CMS’ Hospice Quality Reporting Program includes data submitted directly by hospice providers, from Medicare hospice claims, and from the Hospice Consumer Assessment of Healthcare Providers and Systems survey.
Here are the hospice care quality scores and per-beneficiary spending amounts by state between Jan. 1, 2023, and Dec. 31, 2024, according to CMS:
| State | Hospice Care Index Overall Score | Per-beneficiary spending |
| Alabama | 9.3 | $16,588 |
| Alaska | 8.8 | $13,013 |
| Arizona | 8.8 | $19,693 |
| Arkansas | 9.4 | $14,880 |
| California | 8.3 | $26,927 |
| Colorado | 9.5 | $15,010 |
| Connecticut | 9.6 | $13,702 |
| Delaware | 9.5 | $16,216 |
| District of Columbia | 8.3 | $16,270 |
| Florida | 9.7 | $15,498 |
| Georgia | 8.8 | $17,489 |
| Hawaii | 9.6 | $16,248 |
| Idaho | 9.3 | $15,675 |
| Illinois | 9.1 | $15,181 |
| Indiana | 9.4 | $15,110 |
| Iowa | 9.5 | $11,469 |
| Kansas | 9.1 | $14,806 |
| Kentucky | 9.2 | $8,963 |
| Louisiana | 8.7 | $16,633 |
| Maine | 9.5 | $14,401 |
| Maryland | 9.7 | $12,484 |
| Massachusetts | 9.2 | $17,496 |
| Michigan | 9.0 | $16,300 |
| Minnesota | 9.2 | $15,390 |
| Mississippi | 8.6 | $17,427 |
| Missouri | 9.0 | $14,795 |
| Montana | 8.9 | $11,921 |
| Nebraska | 9.2 | $11,522 |
| Nevada | 8.1 | $21,733 |
| New Hampshire | 9.7 | $14,753 |
| New Jersey | 9.2 | $16,230 |
| New Mexico | 9.0 | $13,829 |
| New York | 9.2 | $11,765 |
| North Carolina | 9.5 | $14,453 |
| North Dakota | 9.3 | $9,600 |
| Ohio | 9.3 | $16,297 |
| Oklahoma | 8.7 | $15,649 |
| Oregon | 9.0 | $14,820 |
| Pennsylvania | 9.0 | $14,102 |
| Rhode Island | 9.8 | $15,028 |
| South Carolina | 9.1 | $16,788 |
| South Dakota | 9.0 | $10,390 |
| Tennessee | 9.6 | $13,528 |
| Texas | 8.4 | $19,852 |
| Utah | 9.2 | $16,794 |
| Vermont | 9.4 | $13,204 |
| Virginia | 9.2 | $14,079 |
| Washington | 9.0 | $13,612 |
| West Virginia | 9.8 | $12,734 |
| Wisconsin | 9.4 | $16,880 |
| Wyoming | 9.2 | $10,410 |
The post Hospice spending, care quality scores by state appeared first on Becker’s Hospital Review | Healthcare News & Analysis.
Michigan system taps AI to flag heart disease risk
Grand Blanc, Mich.-based McLaren Health Care has launched a cardiovascular screening program in partnership with Bunkerhill Health.
The program applies Bunkerhill Health’s AI platform to clinical data from patients’ routine chest CT scans previously performed for other medical reasons, according to a Feb. 18 news release from the health system. The platform’s FDA-cleared algorithms detect and measure incidental coronary artery calcium and aortic valve calcium — indicators of coronary heart disease and aortic stenosis.
McLaren is the first Michigan health system and one of five in the nation to deploy AI-powered aortic valve calcium detection on routine chest CT scans. Bunkerhill Health’s aortic valve calcium algorithm is the first FDA-cleared solution for detecting and evaluating aortic valve calcium in routine chest CT scans, according to the release.
McLaren has begun scanning routine chest CT scans from the past 12 months. The health system said the approach allows it to identify and notify patients for follow-up and preventive care without requiring additional specialized imaging.
The post Michigan system taps AI to flag heart disease risk appeared first on Becker’s Hospital Review | Healthcare News & Analysis.
North Carolina targets PBMs under pricing law
The North Carolina Department of Justice and North Carolina Department of Insurance alerted pharmacy benefit managers Feb. 17 that the state’s SCRIPT Act is now in effect, and said they are prepared to enforce the law.
Attorney General Jeff Jackson and Insurance Commissioner Mike Causey said their offices will work together to ensure fair drug prices and uphold the legislative mandate of the General Assembly, according to a Feb. 17 news release.
The North Carolina General Assembly passed the SCRIPT Act in 2025. The law requires PBMs to allow any pharmacy to participate in their networks and permit patients to use the pharmacy of their choice, pass on most of the savings they negotiate with drugmakers directly to patients, submit annual reports to the North Carolina Department of Insurance and more fairly reimburse independent pharmacies.
The law also gives the Department of Insurance stronger regulatory and enforcement authority and provides the Department of Justice additional authority to enforce North Carolina’s Unfair and Deceptive Trade Practices Act against PBMs. A few PBMs control more than three-fourths of the nation’s 6.6 billion prescription drugs, according to the release.
The post North Carolina targets PBMs under pricing law appeared first on Becker’s Hospital Review | Healthcare News & Analysis.
CVS launches $5M pharmacy scholarship in Louisiana
CVS Health has launched a $5 million scholarship program to support students pursuing a Doctor of Pharmacy degree at Xavier University of Louisiana in New Orleans or the University of Louisiana at Monroe.
The scholarship will open in the 2026-27 academic year, according to a Feb. 18 news release. CVS Health said the scholarship aims to strengthen the pharmacy workforce and expand access to care across the state.
The initiative builds on CVS Health’s broader pharmacy workforce investments. In April 2024, the company unveiled a tuition assistance program allowing PharmD graduates who intern with CVS Pharmacy to apply for up to $20,000 toward their final year of tuition, with plans to expand eligibility to interns in their final two years of pharmacy education. Through a partnership with the American Association of Colleges of Pharmacy, CVS Health also created a community pharmacy health equity scholarship that grants $20,000 to 21 pharmacy students nationwide.
In February 2025, CVS Pharmacy and Duquesne University in Pittsburgh also launched a program offering a 50% tuition scholarship for eligible CVS employees pursuing a Doctor of Pharmacy degree through Duquesne’s online pharmacy program.
The post CVS launches $5M pharmacy scholarship in Louisiana appeared first on Becker’s Hospital Review | Healthcare News & Analysis.

What to Expect When Working for a Nurse Staffing Agency
Starting a new nursing job in metro Atlanta—or anywhere in Georgia, South Carolina, Alabama, Florida or beyond —can feel overwhelming, even when you know it’s the right move. Working for a nurse staffing agency opens the door to exciting opportunities like travel nursing jobs, per diem nursing positions, and flexible contract nursing assignments, but for many nurses, the process can seem mysterious.
Here’s what to expect and how to prepare so you can start your journey with confidence.
Whether you’re interested in contract nursing jobs, per diem, or full-time placements, the process of joining a nursing agency is straightforward.
- Explore Open Positions
Start by browsing our current healthcare staffing opportunities, including travel nurse contracts and per diem RN jobs across Georgia. You can view all available positions [here]. - Apply and Submit Your Resume
Once you find a role that matches your skills and interests—like emergency department nursing jobs, radiology technologist positions, or ICU contract assignments—submit your application. Our recruitment team reviews your resume to ensure a great fit. - Complete Skills Assessments
After initial screening, you’ll complete online assessments to evaluate your clinical expertise. - Interview and Client Screening
Next, you’ll interview with a recruiter from Staff Relief. Some positions require additional interviews with the hiring facility, especially for rapid response nursing or specialized roles.
The good news? This process typically moves fast—most candidates receive an offer within 9 days of applying.
More Earning Potential
One of the biggest reasons nurses choose agencies like Staff Relief is the pay. Per diem and contract nursing jobs can pay up to 50% more than traditional staff positions. You’ll also have access to the same premium assignments available with leading partners such as Aya Healthcare, AMN Healthcare, and Medical Solutions.
More Flexibility and Freedom
When you work with a nurse staffing agency, you decide when and where you want to work. Whether you prefer travel nurse assignments across the Southeast or local shifts around Georgia, you have control over your schedule.
More Responsibility and Professional Growth
As a contract or per diem nurse, you’ll take on additional responsibilities like tracking time and attendance. While this requires organization, it also builds valuable skills in accountability and independence.
More Variety and Travel
You won’t be tied to one facility. With travel nursing jobs, you can explore new cities, gain diverse experience, and enjoy housing assistance coordinated through agency partnerships.
More Security and Benefits
Even though you’re working flexible assignments, you still receive comprehensive benefits. Staff Relief provides health insurance and other perks so you can feel secure in your role.
If you’re a nurse who thrives in a fast-paced, dynamic environment and values more freedom, higher pay, and a variety of assignments, agency work could be your ideal career path.
Staff Relief partners with major healthcare staffing leaders to offer you access to top contracts and exclusive opportunities. Ready to get started?Contact Staff Relief today to learn more about our per diem nursing jobs, travel nurse assignments, and allied health contracts in Georgia. Let the best nurse staffing agency in Geogia find the perfect fit for your skills and goals.

Travel Nurse Pay in Georgia – Updated
Working as a contract nurse or per diem nurse in Georgia opens doors to flexibility, premium pay rates, and the chance to grow your experience across different healthcare settings. Whether you’re comparing travel nursing jobs, exploring remote RN jobs, or looking into per diem nursing positions, it’s essential to understand the factors that impact your earnings so you can make informed decisions and advocate for fair compensation.
Below, you’ll find everything you need to know about travel nurse pay in Georgia, average hourly rates, and how variables like specialty and location shape your paycheck.
When you partner with a nursing staffing agency or medical staffing agency, you’ll likely choose between contract assignments and per diem shifts:
- Contract Nursing Jobs: You’ll sign an agreement to work a set number of hours over a defined period, such as 8–13 weeks. Many contract nursing jobs offer guaranteed hours, premium rates for urgent needs, and stipends for housing and travel.
- Per Diem Nursing Jobs: “Per diem” means “per day.” These shifts are typically scheduled a week at a time, providing maximum flexibility for nurses who prefer short-term or occasional work. Per diem nurses often receive higher hourly rates to compensate for the lack of long-term commitment and benefits.
Whether you’re drawn to the stability of a contract or the freedom of per diem nursing shifts, you’ll be paid hourly, with rates that can fluctuate based on demand and specialty.
No two assignments are exactly the same. Here are the main factors that determine what you’ll earn as a travel nurse or per diem nurse in Georgia:
1. Location
Urban areas like Metro Atlanta and Savannah typically offer higher compensation compared to rural hospitals and clinics. Travel nurse jobs in Atlanta often pay a premium to attract experienced RNs to high-volume facilities.
2. Specialty
Your area of expertise makes a significant difference. Roles in the emergency department, ICU, operating room, and critical care nursing often command the highest hourly rates. Specialized skills like medical imaging, radiology technologist jobs, or dialysis RN contracts can further boost your earning potential.
3. Experience and Credentials
More years in the field—and specialty certifications—qualify you for higher-paying assignments. Rapid response nursing jobs and crisis response contracts also tend to pay more due to urgency and complexity.
4. Facility Type
Pay can vary depending on whether you’re working in an acute care hospital, skilled nursing facility, outpatient clinic, or rehab center. Some settings offer incentives like retention bonuses or completion bonuses.
5. Travel Requirements
Assignments requiring you to commute 50+ miles often include additional stipends or elevated pay rates to offset costs and time away from home.
While rates fluctuate weekly based on demand and season, here’s what you can generally expect in Georgia:
- General RN: $40–$46 per hour
- General RN (Metro Atlanta): $48–$55 per hour
- Specialty RN (ICU, OR, ED): $55–$75+ per hour, depending on urgency and shortage areas
- Licensed Practical Nurse (LPN): $25–$40 per hour
- LPN (Metro Atlanta): $30–$45 per hour
These figures often include travel stipends and housing allowances. For high-paying travel nursing companies or crisis response contracts, rates can exceed $80 per hour in peak demand.
Some agencies bundle housing and travel reimbursements, while others pay a higher hourly rate without stipends.
Before accepting a contract, review details carefully:
- Hourly base pay
- Housing allowance or provided housing
- Meal and incidentals stipends
- Travel reimbursements
- Completion and referral bonuses
If you’re unsure whether a pay package is competitive, compare it with similar contract nursing jobs.
- Get certified in high-demand specialties like emergency room nurse staffing, ICU nursing, or radiology technologist work.
- Consider rapid response nursing or ICU contract nurse positions for premium rates.
- Pick up flexible options like weekend nursing contracts or extra per diem shifts to maximize income.
- Keep your licenses and certifications current to qualify for the broadest range of assignments.
If you’re ready to explore per diem nursing jobs in Georgia or secure a travel nurse contract with competitive pay and benefits, Staff Relief, Inc. is here to help.
Contact us today to learn more about available contracts and start earning what you deserve.

The Ultimate Guide to Per Diem and Travel Nursing Jobs in the Southeast
If you’re an RN exploring your next career move, you’re not alone. Demand for per diem nursing jobs, travel nursing assignments, and contract nursing positions continues to rise across the Southeast—including Georgia, Florida, Alabama, and North Carolina.
At Staff Relief, we specialize in connecting nurses with flexible, rewarding opportunities at top healthcare facilities. Whether you’re searching for remote RN jobs, weekend nursing contracts, or emergency department nursing careers, this guide will help you understand your options and how to get started.
Per diem nursing offers unmatched flexibility. You can pick up shifts on your schedule—ideal for maintaining work-life balance or supplementing your income. Contract nursing jobs, meanwhile, provide stability for a set duration, often with higher pay rates and benefits.
- Flexible nursing shifts that fit your lifestyle
- The ability to work in acute care, skilled nursing facilities, or inpatient care units
- Opportunities to gain experience in critical care, emergency departments, or medical imaging
- Access to rapid response nursing jobs and crisis response travel nurse contracts that offer premium compensation
- The chance to build your resume with respected employers like Aya Healthcare, AMN Healthcare, and Medical Solutions
Many nurses are drawn to the Southeast for its competitive pay and growing healthcare networks. Here are some popular areas to consider:
- Georgia: From Atlanta to Savannah, per diem nursing jobs in Georgia are in high demand. If you’re wondering how to become a travel nurse in Georgia, Staff Relief can guide you through licensing and onboarding.
- Florida: Coastal communities and urban hospitals alike need RNs for contract nursing jobs in Florida, especially in ICU, OR, and emergency room nurse staffing.
- North Carolina: Explore travel nurse assignments in North Carolina, including rapid response nursing and critical care contracts.
- Alabama: More facilities are offering remote RN jobs in Alabama and local contracts to address staffing shortages.
You have more options than ever to search for your next role. While many nurses and allied health professionals look on popular platforms like Indeed and Vivian, applying through multiple agencies can be time-consuming and repetitive.
Staff Relief makes it simpler. Our job board and mobile app put thousands of opportunities in one place. You can browse, compare, and apply to positions without juggling multiple applications or credentialing processes.
Here are a few resources to explore:
- Staff Relief Job Board & Mobile App – Your all-in-one hub for per diem, travel, and contract jobs, with a streamlined application process and dedicated support.
- Indeed – Search a wide range of listings for nursing and allied health jobs.
- Vivian Healthcare Jobs – Compare pay packages and contract details across agencies.
Ready to save time and find your next assignment faster? Start with Staff Relief’s platform for the most efficient experience
Aya Healthcare, AMN Healthcare, and Medical Solutions are some of the most respected companies in the industry offering extensive travel nursing, per diem, and rapid response assignments nationwide. As a partner, Staff Relief has access to some of the same contracts and exclusive opportunities available through Aya, AMN, and Medical Solutions. You can explore top-paying positions without having to apply separately to multiple agencies. Whether you’re interested in Aya Healthcare contracts, AMN Healthcare rapid response nursing jobs, or Medical Solutions travel nurse assignments, our team can help you compare options and secure the role that fits you best.
Choosing the right nursing agency is essential. Whether you’re evaluating Aya Healthcare reviews, AMN Healthcare pay packages, or Medical Solutions job openings, here are factors to consider:
- Transparent pay packages and benefits
- Support with licensing and credentialing
- Access to crisis response contracts and rapid response nursing jobs
- A reputation for placing nurses in top paying travel nursing companies
- Ongoing support and career development resources
Staff Relief partners with major systems and local facilities to deliver healthcare staffing solutions that prioritize both the nurse and the patient.
If you’re searching for flexible RN shifts, contract nursing jobs, or remote nursing positions, we’re here to help. From emergency department nurse jobs to radiology technologist staffing, our team can match you with assignments that fit your goals.
Connect with Staff Relief today to get personalized recommendations, compare contracts, and start your next chapter with confidence.

Pros and Cons for Working for a Nurse Staffing Agency
In today’s fast-changing healthcare landscape, more nurses are exploring flexible career paths, including per diem nursing jobs, travel nursing contracts, and remote RN positions. Whether you’re a seasoned nurse searching for higher pay or a new grad eager to explore diverse settings, working with a nursing staffing agency can be a rewarding option. But like any career move, it’s important to weigh the benefits and challenges before deciding.
Below, we break down the main pros and cons of working with a medical staffing agency in Georgia and across the Southeast, so you can make the best choice for your lifestyle and goals.
One of the top reasons nurses choose per diem nursing positions or local contract nursing is the freedom to control their schedule. Unlike full-time hospital roles, contract assignments and per diem shifts let you decide when and where you work. This flexibility is ideal if you have family commitments, are pursuing further education, or simply want more autonomy in your day-to-day life.
Agencies like Aya Healthcare, AMN Healthcare, and Medical Solutions often post weekend nursing contracts, PRN RN positions, and rapid response nursing jobs you can pick up on your terms.
If maximizing your earnings is a priority, you’ll be glad to know that contract nursing jobs and per diem shifts typically pay higher hourly rates compared to permanent staff roles. These assignments often include stipends for meals, lodging, and travel—especially for travel nurse jobs in Atlanta, Savannah, and the Florida Panhandle. Many nurses find that with smart budgeting; they can work fewer shifts while maintaining or even increasing their income.
Plus, expenses related to travel nursing—like transportation and temporary housing—are often tax-deductible, creating additional financial benefits.
For nurses who thrive on change, working with a healthcare staffing agency provides a steady stream of new experiences. You’ll build your skills across different units, such as emergency departments, inpatient care, and even specialized areas like radiology technologist jobs or diagnostic imaging. This variety not only helps you stay engaged but also makes your resume stand out to future employers.
While flexible shifts are a major perk, it’s important to recognize that per diem nursing jobs don’t always guarantee steady hours. You may have weeks packed with back-to-back assignments, followed by slower periods. In some cases, last-minute schedule changes can impact your plans. If you prefer consistency, consider long-term contract nursing jobs, which often range from 6 to 17 weeks and offer more predictable schedules.
Contract and travel nurses frequently rotate among facilities, from skilled nursing facilities to acute care hospitals. Each location has its own protocols, electronic health records, and workplace culture. While you’ll eventually become comfortable in new settings, the learning curve can feel steep, especially when starting out. Nurses who value long-term relationships with coworkers and patients may find this aspect challenging.
If you’re adaptable, resourceful, and excited by the idea of working in diverse environments, you’re well-positioned to succeed. Many RNs say contract work rekindled their passion for patient care, exposed them to innovative treatments, and expanded their professional networks.
Whether you’re interested in remote nursing jobs in Alabama, ICU travel nurse assignments in Georgia, or emergency room contracts throughout the Southeast, there’s no shortage of options through reputable agencies like Aya Healthcare, AMN Healthcare, and Medical Solutions.
Ready to explore per diem nursing positions or contract opportunities? Here are a few steps to begin:
- Research Top Agencies: Read reviews and compare pay packages, benefits, and housing support.
- Set Your Priorities: Decide what matters most—schedule flexibility, pay rate, location, or specialty.
- Prepare Documentation: Update your licenses, certifications, and resume.
- Search Nursing Jobs Online: Use platforms like Indeed, Vivian Health, and agency job boards to find assignments that match your goals.
- Ask Questions: Speak with recruiters to understand expectations, cancellation policies, and support resources.
Working with a nursing staffing agency can be an empowering way to build a flexible, well-paid, and fulfilling career. If you’re considering making a change, take time to explore your options and connect with agencies committed to supporting nurses at every step.
Explore current per diem and contract openings with Staff Relief today and discover how flexible nursing can work for you.

How to Get a High Paying Contract Nursing Job
Contract nursing offers the chance to do meaningful work, gain diverse experience, and earn competitive pay. Whether you’re pursuing contract nursing jobs, per diem nursing positions, or rapid response assignments, the key to maximizing your income is preparation and strategy.
If you’re ready to secure a high-paying contract nursing job, use these proven tips to set yourself apart and negotiate pay that reflects your expertise.
Your resume is your first impression. A clear, polished resume highlights your skills, certifications, and professional accomplishments, and it determines whether you’ll be invited to interview.
Include:
- Your nursing specialties (such as ICU, emergency department, or medical imaging)
- Certifications (like ACLS, BLS, or specialty credentials)
- Details about your experience in different care settings, such as inpatient care, skilled nursing facilities, or acute care staffing
It’s normal to have employment gaps but be ready to confidently explain them during interviews. A well-organized resume positions you as a serious professional ready for high-paying nursing contracts.
Keeping your credentials updated makes you a more attractive candidate and can improve your earning potential.
Make sure to:
- Renew essential licenses and certifications promptly.
- Consider adding specialty certifications that are in demand for travel nursing jobs and contract assignments.
- Stay up to date with immunizations required by hospitals and clinics. Being ready with all documentation can speed up onboarding and help you access crisis response nursing jobs or urgent needs contracts that often pay premium rates.
The more prepared you are, the easier it is for a nurse staffing agency or recruiter to match you with higher-paying positions.
Professional references can be the deciding factor in landing a top-paying assignment.
Employers and recruiters rely on references to verify your:
- Clinical skills
- Professionalism
- Reliability
Choose references who can confidently speak to your work ethic and performance. Positive recommendations can open the door to flexible nursing shifts, per diem contracts, and specialized roles that pay more.
Flexibility is often rewarded in the world of contract nursing.
Consider these options to boost your pay:
- Accepting night shifts or weekends, which usually come with higher hourly rates.
- Taking assignments in locations experiencing shortages, such as rural facilities or emergency department nursing jobs.
- Being open to rapid response contracts or crisis response assignments, which often offer premium compensation.
When you demonstrate a willingness to adapt, you make yourself more valuable to medical staffing agencies and healthcare employers.
In contract nursing, your reputation follows you from one facility to the next. A strong track record makes it easier to secure higher-paying contracts and preferred assignments.
Tips for maintaining a great reputation:
- Be punctual and dependable.
- Communicate clearly with staffing agencies and supervisors.
- Go the extra mile to provide excellent patient care.
Facilities are willing to pay more to bring on nurses with proven reputations for excellence.
Being a contract nurse offers countless benefits, from career variety to premium pay. To make the most of your opportunities:
- Invest time in preparing a strong resume.
- Keep certifications and immunizations current.
- Maintain excellent references.
- Stay flexible with shifts and assignments.
- Build and protect your professional reputation.
When you combine preparation with dedication, you can consistently secure high-paying contract nursing jobs that match your skills and goals.
If you’re looking for your next opportunity, Staff Relief, Inc. is here to help. We partner with hospitals, clinics, and healthcare facilities to connect nurses with the best assignments in Georgia and beyond.
Contact us today to explore available contracts and start earning what you deserve.

How to Find the Best Nursing and Allied Health Jobs in 2025
If you’re thinking about a career change this year, you’re not alone. Thousands of nurses and allied health professionals are exploring contract nursing, per diem shifts, and even remote RN jobs to gain more flexibility, better pay, and fresh experiences.
But with so many options and so many staffing agencies—how do you know where to start?
This guide will walk you through:
✅ Why more professionals are choosing contract and per diem work
✅ How to evaluate agencies and read nursing agency reviews
✅ Where to find the best nursing jobs in 2025
✅ Tips for comparing assignments and getting hired faster
The days of sticking to one hospital job for your entire career are long gone. Today’s nurses are building more dynamic, customized careers—often combining contract assignments with per diem shifts.
The benefits of contract nursing are clear:
- Higher pay compared to permanent staff roles
- Housing and travel stipends
- Bonuses for completing assignments
- The chance to build experience in specialized areas like ICU, ER, and diagnostic imaging
- Flexibility to take time off between contracts
Meanwhile, per diem nursing jobs offer even more control over your schedule. You can pick up shifts when you want—whether that means extra weekends or just a few days a month.
If you’re drawn to this flexibility, you’re in good company. Contract and per diem work have become the fastest-growing segments of healthcare employment.
Once you decide to make a change, your next step is choosing a partner to help you find assignments. But not all agencies are the same.
Before you commit, take time to read nursing agency reviews. Here’s what to look for:
- Transparency in pay packages and benefits
- Support with licensing, credentialing, and onboarding
- Access to rapid response nursing jobs and high-demand contracts
- A track record of placing candidates in the highest paying travel nursing companies
- Clear communication and responsive recruiters
At Staff Relief, we know that trust matters. As a partner of Aya Healthcare, AMN Healthcare, and Medical Solutions, we can give you access to exclusive contracts without the hassle of applying to multiple platforms.
There are dozens of websites that list healthcare jobs, but it’s easy to get overwhelmed. To save time, start with the best nursing job sites for 2025:
- Staff Relief Job Board & Mobile App – Your one-stop platform to see per diem, contract, and travel nursing jobs nationwide, including remote RN jobs and medical imaging positions.
While many agencies focus on nursing alone, allied health roles are booming, too. If you’re a technologist or imaging specialist, consider exploring:
- Radiology technologist jobs in hospitals and outpatient centers
- Diagnostic imaging careers in high-demand specialties
- Medical imaging staffing agencies that can connect you to flexible contracts
- Radiographer employment for mobile imaging services or large health systems
Staff Relief supports professionals across disciplines and can help you find medical imaging jobs near you with excellent pay and benefits.
Ready to pick up extra shifts or transition into per diem work full-time? Here are tips to get per diem nursing jobs faster:
- Keep your credentials and health records updated.
- Sign up with an agency that has real-time job listings.
- Use the Staff Relief app to get instant alerts when new shifts are posted.
- Be proactive—per diem openings often fill quickly.
Whether you want the best remote nursing jobs for RNs, the stability of contract work, or the variety of per diem assignments, 2025 is the perfect year to take control of your career.
At Staff Relief, we make it easy to:
- Access the highest paying travel nursing companies
- Compare contracts side by side
- Read verified nursing agency reviews
- Secure opportunities in radiology, imaging, and allied health
- Apply once and explore thousands of jobs nationwide
Connect with Staff Relief today, and let’s build your path forward together.

Everything You Need to Know About Travel Nurse Credentialing
Every hospital, clinic, and long-term care facility has its own standards for verifying a clinician’s qualifications and readiness to practice. Even if you’ve worked at a similar facility before, you can’t automatically carry over your credentials. Each assignment requires you to complete a credentialing and onboarding process to ensure patient safety and compliance with regulations.
Credentialing typically includes:
- Drug screening
- Health assessments
- Proof of licensure and certifications
- Background checks and reference verifications
- Competency exams
- Facility-specific training and onboarding
Many nurse managers or department leaders will schedule a phone or video call to review workflows, discuss expectations, and confirm you’ve completed all requirements before your start date.
Preparation is key. Keeping all your essential documents organized will save you time and stress whenever you accept a new assignment. Here’s what you’ll need to have ready:
- Copies of your professional license(s) and any specialty certifications (such as BLS, ACLS, PALS)
- Two valid forms of identification (e.g., driver’s license and passport)
- A record of your annual physical exam (valid for one year)
- TB test results (valid for one year)
- Drug screen results
- Immunization and titer records (MMR, Varicella, Hepatitis B, and others)
- Proof of flu vaccination (especially if starting in the fall or winter)
- COVID vaccination records if required by the facility
- Payroll forms and direct deposit information
- References and verified work history
- Competency test results (if applicable)
If you want to avoid delays, consider getting your TB test, physical, and immunizations updated while you’re applying for contracts. Staying current helps you move quickly when the right opportunity arises.
Most healthcare facilities require online assessments to verify your competency in your specialty. These assessments might include:
- Skills checklists
- Clinical scenario testing
- Electronic medical record (EMR) training modules
Once you pass these evaluations, you’ll typically complete one to two days of orientation to get familiar with the facility’s policies, documentation standards, and workflows. This process helps ensure you can provide safe, effective care from day one.
If you work in in-demand roles such as ER RN, PCU RN, CT Technologist, RRT, Surgical Tech, Mammo Tech, Home Health RN, or M/S RN, expect additional verifications and specialty-specific assessments. Facilities often have strict guidelines for these positions due to the complexity of care and the need for current certifications.
Staff Relief’s credentialing team can walk you through these specialty requirements step by step so you feel confident and prepared.
Large national agencies often have more rigid, self-directed credentialing processes. Working with a regional partner like Staff Relief provides you with hands-on support. Our team will:
- Help you track deadlines for documents and assessments
- Coordinate background checks and health screenings
- Connect you with local resources for TB testing and physicals
- Answer your questions about compliance and onboarding
This personal guidance ensures nothing falls through the cracks—and you’re always ready to step into your next assignment.
Credentialing isn’t a one-time process. Here are a few habits that can help you stay organized:
- Keep a digital folder with scanned copies of your documents
- Mark your calendar with expiration dates for your TB test, physical, and certifications
- Get your annual flu shot early if you expect to start an assignment in the fall
- Check whether your next facility requires a COVID vaccine or booster
- Keep your immunizations up to date to avoid delays
Being proactive makes you more competitive for premium travel contracts and quick-start assignments.
Navigating credentialing can feel like a lot to manage, especially if you’re juggling multiple offers. That’s why choosing the right staffing partner is so important.
Staff Relief has years of experience supporting clinicians across Georgia, Alabama, Florida, and the Carolinas. Whether you’re a first-time traveler or a seasoned professional, you’ll have a dedicated team behind you to make credentialing smooth, transparent, and stress-free.
If you’re exploring travel nursing jobs or allied health contracts in the Southeast, our team is here to help you navigate credentialing and start your next adventure with confidence. Contact Staff Relief today to learn about current opportunities and get expert support every step of the way.

Addressing Georgia’s Critical Nursing Shortage
The nursing shortage in Georgia has reached critical levels in 2025, with nearly every county—urban and rural—struggling to recruit and retain qualified healthcare professionals. This crisis isn’t just about open positions; it’s about ensuring patients receive safe, timely, and compassionate care when they need it most.
From major hospitals to long-term care facilities, healthcare organizations are urgently seeking skilled nurses, surgical techs, and allied health professionals who can step into high-demand roles and make an impact.
Several factors continue to drive Georgia’s nursing shortage:
- Rising demand for healthcare services: The state’s aging population and expanded access to care have increased the need for RNs, LPNs, and allied health professionals.
- Burnout and workforce attrition: The lingering effects of the pandemic, combined with long hours and emotional stress, are pushing many clinicians to reduce hours, retire early, or leave the field altogether.
- Education and training bottlenecks: Limited capacity in nursing schools and faculty shortages continue to constrain the pipeline of new graduates.
- Rural disparities: Non-metro counties face even steeper challenges recruiting clinicians, leaving communities with limited access to primary and specialty care.
As a result, many hospitals and clinics are leaning heavily on travel contracts, per diem staff, and flexible assignments to keep up with patient needs.
The staffing shortage has ripple effects throughout Georgia’s healthcare infrastructure:
- Hospitals are relying on travel clinicians—especially in specialties like ER RNs, PCU RNs, and Surgical Techs—to fill critical gaps.
- Skilled professionals such as CT Technologists, RRTs, Mammo Techs, and Home Health RNs remain in high demand, driving up competition and pay rates.
- Burnout among the remaining workforce leads to higher turnover, further deepening shortages.
- Patients experience longer wait times, delayed procedures, and uneven access to care, particularly in rural and underserved areas.
The result is a cycle of strain that requires strategic intervention.
While the challenges are significant, Georgia’s healthcare leaders are adopting innovative strategies to rebuild the workforce and improve retention:
1. Expanding Educational Pathways
- New state investments in nursing schools and allied health programs are increasing enrollment capacity.
- Fast-track bridge programs are helping LPNs and paramedics advance to RN licensure more efficiently.
2. Financial Incentives and Career Support
- Loan repayment and tuition reimbursement programs are helping attract graduates to high-need areas.
- Retention bonuses and flexible scheduling are becoming standard in many contracts.
3. Investing in Burnout Prevention
- More facilities are offering mental health resources and dedicated time off to protect clinician well-being.
- AI-supported scheduling tools are helping balance workloads and reduce last-minute staffing gaps.
4. Expanding Telehealth and Remote Care
- Telehealth adoption continues to grow in 2025, allowing clinicians to manage certain care remotely.
- Hybrid care models are easing staffing pressures in rural counties.
5. Embracing Flexible Staffing Models
- Short-term contracts, rapid response assignments, and per diem shifts give clinicians more options to work on their terms.
- Many clinicians are finding that a mix of travel and local assignments offers better work-life balance.
Healthcare facilities across Georgia and the Southeast increasingly rely on experienced staffing agencies to fill urgent and specialized positions. When you partner with a staffing agency that understands the local landscape, you gain access to:
- Skilled clinicians ready to step into critical roles—whether it’s an ER RN, PCU RN, CT Tech, RRT, or Mammo Tech.
- Flexible workforce solutions to manage seasonal demand and unexpected absences.
- Streamlined credentialing and onboarding to get staff in place faster.
- Insights into regional pay trends and incentives.
Staff Relief, for example, has built long-standing partnerships with hospitals, outpatient centers, and home health agencies across Georgia, Florida, Alabama, and the Carolinas, making it easier to adapt to changing needs.
If you’re considering your next step in nursing or allied health, there has never been a better time to explore opportunities in Georgia. Clinicians with experience in specialties like emergency nursing, progressive care, surgical services, medical-surgical units, and diagnostic imaging are in especially high demand.
With flexible contracts, competitive compensation, and support from experienced recruiters, you can build a career that aligns with your goals and helps meet a pressing need.
Georgia’s nursing shortage is a complex, urgent issue—but progress is happening. By investing in education, supporting the workforce, embracing innovation, and building strong partnerships, the state is working to rebuild its healthcare capacity.
If you’re a healthcare professional ready to make an impact—or a facility seeking experienced clinicians—this is the moment to take action.
Ready to explore the latest opportunities or learn how strategic staffing can help? Contact Staff Relief today and join the effort to strengthen Georgia’s healthcare system for everyone.

10 Tips for Travel Nurses
Travel healthcare is more than just an assignment, it’s an opportunity to expand your skills, explore new places, and make an impact where it matters most. Whether you’re a seasoned travel nurse, a respiratory therapist, or a surgical technologist, knowing how to navigate contracts and maximize your experience is key to success.
Here are ten essential tips every travel healthcare professional should keep in mind.
1. The Demand for Your Skills is Higher Than Ever
In 2025, healthcare facilities across the Southeast in Georgia, Alabama, Florida, and the Carolinas are experiencing critical staffing shortages. High-demand specialties like CT Tech, ER RN, Surgical Tech, RRT, PCU RN, Mammo Tech, Home Health RN, and M/S RN are seeing unprecedented opportunities.
Travel nursing jobs and allied health contracts are plentiful, but competition can be fierce for the best assignments. Staying flexible and proactive will help you secure roles that match your expertise and goals.
2. Understand Tax Implications of Travel Assignments
Many clinicians overlook how travel pay affects their taxes. Housing stipends, travel reimbursements, and per diem allowances can all impact your taxable income. It’s wise to consult a tax professional who understands healthcare contracts to ensure you’re planning ahead and taking advantage of eligible deductions.
3. Credentialing and Compliance Take Preparation
Every state has different licensure and credentialing requirements. Georgia, Florida, and the Carolinas all have their own rules around background checks and health records.
Be prepared to provide:
- A TB test (valid for 1 year)
- A current physical exam (valid for 1 year)
- Titers and immunization records
- A background check
- A drug screen
It’s smart to get your TB test, physical, and immunizations done while you’re applying so you’re ready as soon as you receive an offer. Keep your immunizations updated, including your flu shot in the fall and COVID vaccinations where required. This will prevent delays when it’s time to start your contract.
Working with a healthcare staffing agency like Staff Relief ensures you’ll have help coordinating these documents and understanding what’s required for each facility.
4. Housing Options Vary by Assignment
Some contracts include housing stipends, while others offer pre-arranged accommodations. It’s critical to understand:
- What your stipend covers
- Whether you’ll be responsible for utilities, deposits, or furniture
- How your housing affects your taxable income
If you prefer to find your own place, Staff Relief can help source local housing options and connect you to reputable providers in your assignment area.
5. Your Reputation Will Follow You
Healthcare facilities often work with the same staffing partners across regions. Showing up on time, being adaptable, and maintaining professionalism will build your reputation and make it easier to secure future assignments.
Positive references can help you access competitive roles in specialties like ER, PCU, and surgical services.
6. Flexibility is Your Superpower
The most successful travel clinicians are those who can pivot quickly. Being open to night shifts, rural contracts, or high-demand specialties often results in higher pay and priority placement.
If you’re willing to work in critical areas, you’ll find more opportunities and stronger negotiating power.
7. Pay Packages Can Be Complex
Your compensation may include:
- Base hourly pay
- Travel stipends
- Housing allowances
- Completion bonuses
Make sure you understand the full picture, not just the hourly rate. This is essential so that you can budget effectively. A reputable healthcare staffing agency will always be transparent about how your pay is structured.
8. Burnout is Real so Take Care of Yourself
Long shifts and adapting to new teams can be stressful. Protect your mental health by:
- Scheduling regular downtime between contracts
- Accessing telehealth services offered through Staff Relief for confidential support
- Staying connected to your support network
Prioritizing self-care helps you bring your best to every assignment.
9. Smaller Agencies Can Get You Into Hidden-Gem Facilities
Smaller agencies can often place clinicians into smaller community hospitals and rural facilities where patient loads are more manageable, but pay rates remain competitive. These positions are available through Staff Relief in Georgia, Alabama, and South Carolina. Only Staff Relief and one or two other boutique firms serve these facilities, so you won’t find these assignments through large national agencies like Aya, Medical Solutions, or AMN Healthcare.
10. Choosing the Right Staffing Partner Matters
Your agency isn’t just your employer, it’s your advocate. The best healthcare staffing partners:
- Have deep relationships with respected hospitals and clinics
- Offer personal support before, during, and after your assignment
Staff Relief has decades of experience supporting clinicians across the Southeast, combining local expertise with a commitment to transparency and respect.
If you’re exploring travel nursing jobs or allied health contracts in Georgia and beyond, now is the time to take the next step. With the right support and preparation, your travel career can be rewarding, sustainable, and full of growth. Contact Staff Relief today to learn about current opportunities and find the right fit for your skills and goals.

How to Choosing the Right Medical Staffing Agency
Choosing the right medical staffing agency isn’t just about finding a job—it’s about building a career with the support, transparency, and opportunities you deserve. Whether you’re looking for contract nursing jobs, travel assignments, or allied health positions, partnering with the right agency helps you feel confident every step of the way.
As a regional leader in the Southeast serving Georgia, the Carolinas, Alabama, and Florida, Staff Relief specializes in high-demand roles and offers deep local expertise to help you succeed.
Here are six essential tips to guide your search for a medical staffing agency you can trust.
1. Work with a Partner Who Knows the Region
When you’re working in states across the Southeast, you want an agency that understands the unique dynamics of each market. Regional experience matters because:
- Different states have varying credentialing and compliance requirements
- Compensation rates shift between urban and rural facilities
- Each area has its own demand for specialties, including CT Tech, ER RN, Surgical Tech, RRT, PCU RN, Mammo Tech, Home Health RN, and M/S RN assignments
Staff Relief’s recruiters have years of experience placing clinicians throughout Georgia, Alabama, Florida, and the Carolinas. This local knowledge ensures you’re matched with facilities that fit your skills, preferences, and professional goals.
2. Evaluate the Agency’s Reputation and Track Record
A medical staffing agency’s history is a strong indicator of what you can expect. Take time to:
- Explore the agency’s website to see testimonials from nurses, surgical techs, respiratory therapists, and imaging professionals
- Review social media and online platforms for authentic feedback
- Look for examples of long-term partnerships with respected hospitals, outpatient centers, and home health organizations across the Southeast
When you choose an agency that has established relationships and a reputation for consistency, you gain peace of mind that your career is in capable hands.
3. Expect Clear Communication About Pay
Transparency around compensation is crucial. Medical staffing pay packages can include:
- Base hourly rates
- Travel and housing stipends
- Bonuses
Without clarity, it’s easy to feel uncertain about what you’ll actually earn. A trustworthy agency will explain exactly how your pay is structured, whether you’re taking on a rapid response ER RN contract, a CT Tech travel assignment, or a Mammo Tech position.
At Staff Relief, we prioritize transparent communication so you can make informed decisions and feel confident in your earnings.
4. Assess Benefits and Support
The right staffing agency offers more than just placements. Look for a partner that provides:
- Credentialing and compliance support
- Guidance navigating state requirements if you’re crossing from Georgia into Florida, Alabama, or the Carolinas
- Professional development resources and scheduling assistance
Staff Relief is committed to offering comprehensive support, so you can focus on providing excellent patient care, whether you’re working in PCU, ER, surgical services, or home health.
5. Look for Joint Commission Certification
When an agency is Health Care Staffing certified by The Joint Commission, it demonstrates a commitment to quality and safety. Certification means the agency has:
- Passed rigorous evaluations of processes, compliance, and clinical standards
- Demonstrated consistent excellence in recruiting and supporting healthcare professionals
This recognition shows you’re working with an organization that meets the highest standards. This is something you can expect when partnering with Staff Relief.
6. Find the Right Fit for Your Working Style
Every agency operates differently. Some rely on automated platforms and self-service tools, while others offer more personal, one-on-one support.
Ask yourself:
- Do you want direct access to a recruiter who knows you by name?
- Would you rather work with an agency that manages credentialing and logistics for you?
- Do you prefer a more high-touch approach over an impersonal online process?
Choosing an agency that fits your communication style and values makes every assignment more rewarding. Staff Relief’s approach is personal, responsive, and focused on helping you thrive in the role that’s right for you.
When you work in specialized, high-demand fields like CT Tech, ER RN, Surgical Tech, RRT, Mammo Tech, PCU RN, Home Health RN, and M/S RN. You deserve a staffing partner who understands your expertise and advocates for your success.
The right agency combines:
- Regional knowledge of healthcare employers throughout Georgia, Alabama, Florida, and the Carolinas
- Transparent, competitive pay structures
- Robust support and credentialing assistance
- A proven reputation with hospitals and clinics across the Southeast
- Certification that demonstrates credibility
- A commitment to personal service and professional respect
With the right support you’re not just taking a job, you’re building a sustainable career.
If you’re exploring your next contract or travel assignment in the Southeast, Staff Relief is here to help. Our partnerships with respected healthcare facilities and our experience placing clinicians in high-demand specialties mean you can feel confident you’re making the best move for your future.
Contact us today to learn more about available positions and start your search with a staffing agency that puts you first.

The Cost of Nurse Turnover: A Breakdown
Poor nurse retention is a major issue for healthcare facilities, with the national registered nurse (RN) turnover rate standing at nearly 20%. According to the 2024 NSI National Healthcare Retention and RN Staffing Report, the average cost of nurse turnover is estimated to be $56,300 per every RN who leaves their job. For the average hospital, this can equate to roughly $3.9 to $5.8 million in losses per year.
Beyond the financial impacts, high turnover can also have rippling effects on company culture and patient care. In this article, we’ll break down all the costs of nurse turnover and outline strategies that can help you mitigate this issue at your facility.
Nurse turnover occurs when nursing professionals leave their jobs or the profession altogether. This can include instances in which staff are involuntarily terminated from their positions, enter retirement, or choose to leave their roles for other reasons. Some of the most common reasons why nursing professionals willingly leave their jobs include burnout, feeling underappreciated, and a lack of peer support.
Before we break down the cost of nursing turnover, it’s important to note that national nurse turnover and cost estimates often only account for RNs. While it’s difficult to estimate a turnover rate that is representative of all levels of nursing, let’s take a look at how turnover rates and costs have been reported for other types of roles:
- The cost of nurse practitioner turnover is estimated to be $85,832 to $114,919 per episode, with the average turnover rate standing at roughly 10%.
- The cost of nurse managerturnover is estimated to be between $132,00 to $228,000 per episode, with some hospitals reporting that 50% of their nurse leaders intend to leave their jobs within 5 years.
- The indirect costs of replacing one certified nursing assistant (CNA) can range from $3,000 to $6,000, with turnover rates averaging as high as 50% in nursing homes alone.
From these statistics, it’s clear that turnover costs can add up quickly if nursing professionals keep leaving their positions. But how exactly does turnover amount to millions of dollars per year? Here’s a rundown of what can contribute to both the economic and non-economic costs.
There are several ways in which frequent turnover can lead to increased operational costs for facilities. We’ll review and summarize these costs below.
Costs of Vacancies
When a nurse leaves their position, facilities must spend excess money to compensate for vacancies and understaffing. This includes the costs of advertising the opening, hiring temporary staff, and paying existing staff for overtime. Facilities may even need to close beds and defer patients, which leads to diminishing returns.
Several studies have found that these factors combined can contribute to significant losses, accounting for anywhere between 44% to 83% of turnover costs. These costs also continue to rise the longer a position stays open.
Costs of Training
Each time a facility hires a new nurse, additional resources must be spent for onboarding and training. Research has suggested that training can account for roughly 7% to 9% of turnover costs, as preceptors are often given temporary salary raises to orient new nurses.
Facilities that invest in new nurse residency programs are also estimated to incur an additional training cost of roughly $2,041 per resident. Residency programs are often used as a strategy to improve new nurse retention. But if turnover remains high for other reasons, these programs can have a lower return on investment.
Costs of Productivity Loss
Studies have also shown that initial reductions in productivity can contribute to a large proportion of losses, accounting for roughly 45% to 88% of turnover costs. This is because facilities are essentially paying two nurses to do the work of one during training periods — with some preceptorships lasting months at a time.
Additionally, there can be variations in skill level when facilities use a mix of temporary staff. This means that managers may need to spend more time overseeing care, which also contributes to reduced productivity at the leadership level.
High turnover can also impact the overall workflow and culture at a facility. These non-economic costs are important to consider since they can, conversely, lead to more turnover and create a cyclical issue over time.
Poor Teamwork
High turnover means that the entire nursing team must frequently adapt to new personalities and workstyles. Studies have shown that this can worsen communication and collaboration, impacting the overall cohesiveness of the unit. This can also make it more difficult to retain new hires, since teams may come across as unsupportive.
Lower Quality of Care
When existing staff take on increased workloads to compensate for gaps in staffing, quality of care can go down. Some studies have even shown that high turnover can significantly increase the rate of medical errors, mortality, pressure ulcers, and length of stay.
Reduced Employee Morale
The fragmented communication and increased stress resulting from high turnover can also lower staff morale. This may contribute to burnout, which can cause even more nurses to leave their jobs if staff retention and job satisfaction aren’t made a priority.
While there are many different causes of nurse turnover, studies have shown that nurses are four times more likely to voluntarily leave their positions than to get involuntarily terminated. This means that comprehensive measures at the institutional level are needed to retain staff and keep them satisfied in their roles.
Fundamentally, it’s important to engage your staff in conversations and identify the root causes of turnover at your facility. From there, you can apply more meaningful solutions that help your staff feel supported. This may include:
- Using sustainable staffing alternatives that allow for manageable workloads.
- Empowering nurses by giving them more control over their schedules and work.
- Creating a healthy work environment to prevent staff burnout.
- Providing transparent, consistent, and objective leadership.
The cost of nurse turnover can impact the operations, care quality, and culture at your facility. Need solutions that will stabilize your workforce in the long run? Get dozens of free, expert-written facility management tips and insights delivered straight to your inbox.
https://www.intelycare.com/facilities/resources/the-cost-of-nurse-turnover-a-breakdown/
KPMG’s 2017 U.S. Hospital Nursing: Labor Costs Study
This study identifies several trends and benchmarks in relation to hospital nursing labor costs in the United States. Some of the key findings are summarized below. When all costs are considered, traveling nurses appear to cost less than permanent nurses on an hourly basis. Cost data provided by hospitals indicates that the hourly, all-in cost for a full-time, permanent nurse is approximately $89. This hourly cost is higher than traveling nurses that cost approximately $83 per hour. Key costs that are after captured in this all-in measure are overtime pay, paid time off, retirement, insurance, recruiting, and payroll taxes – and these costs vary by nurse type. Additionally, the survey finds a quantifiable “hidden” cost associated with permanent nurses that is the result of non-productive labor hours, and an unquantified “hidden” cost associated with attrition and time required to fill a permanent direct care registered nurse position. Respondents to the survey indicated that traveling nurses are widely used today, representing approximately 11 % of respondent’s nursing staffs. Also, these hospitals indicated their use of traveling nurses will likely continue to grow in the future. Primary factors for this upward trend are local nursing shortages and facility growth. In all, traveling nurses appear to be a cost effective source of labor tor hospitals, and hospitals are forecasting higher usage of these nurses in the future.

2025 NSI National Health Care Retention & RN Staffing Report
With people living longer, the subsequent rise in chronic conditions and the fact that all Baby Boomers will reach retirement age by 2030, recruiting and retaining quality staff will continue to be a top healthcare issue for years to come. Last year, hospitals increased staff by adding ~304,000 employees, a 5.4% add rate. Of this, ~98,000 RNs were hired which represents a 5.6% RN add rate.
Hospital and RN turnover continue to fall but both remain slightly elevated. Nationally, the hospital turnover rate stands at 18.3%, a 2.4% decrease from CY23, and RN turnover is recorded at 16.4%, a 2.0% decrease. Registered Nurses working in pediatrics, women’s health, and surgical services reported the lowest turnover rate, while nurses working in behavior health, step down and emergency services experienced the highest.
The cost of turnover can have a profound impact on diminishing hospital margins and needs to be managed. According to the survey, the average cost of turnover for a bedside RN is $61,110, an 8.6% increase, resulting in the average hospital losing between $3.9m – $5.7m. Each percent change in RN turnover will cost/save the average hospital an additional $289,000/yr.
The RN vacancy rate also remains elevated at 9.6% nationally. While 0.3% lower than last year, over forty percent (41.8%) reported a vacancy rate of ten percent or more. The RN Recruitment Difficulty Index decreased three (3) days to an average of 83 days. In essence, it takes approximately 3 months to recruit an experienced RN, with step down and med/surg presenting the greatest challenges. Feeling financial stress, hospitals will continue to focus on controlling the high cost of labor with contract labor being a top strategy to navigate a staffing shortage. The greatest potential to offset margin compression is in the top budget line item (labor expense). Every RN hired saves $79,100. An NSI contract to replace 20 travel nurses could save your institution $1,582,000.
2024 Employer Health Benefits Survey
Employer-sponsored insurance covers 154 million nonelderly people. To provide a current snapshot of employer sponsored health benefits, KFF conducts an annual survey of private and non-federal public employers with three or more workers. This is the 26th Employer Health Benefits Survey (EHBS) and reflects employer-sponsored health benefits in 2024.

Hiring More Nurses Generates Revenue for Hospitals
Underfunding is driving an acute shortage of trained nurses in hospitals and care facilities in the United States. It is the worst such shortage in more than four decades. One estimate from the American Hospital Association puts the deficit north of one million. Meanwhile, a recent survey by recruitment specialist AMN Healthcare suggests that 900,000 more nurses will drop out of the workforce by 2027.
American nurses are quitting in droves, thanks to low pay and burnout as understaffing increases individual workload. This is bad news for patient outcomes. Nurses are estimated to have eight times more routine contact with patients than physicians. They shoulder the bulk of all responsibility in terms of diagnostic data collection, treatment plans, and clinical reporting. As a result, understaffing is linked to a slew of serious problems, among them increased wait times for patients in care, post-operative infections, readmission rates, and patient mortality—all of which are on the rise across the U.S.
Tackling this crisis is challenging because of how nursing services are reimbursed. Most hospitals operate a payment system where services are paid for separately. Physician services are billed as separate line items, making them a revenue generator for the hospitals that employ them. But under Medicare, nursing services are charged as part of a fixed room and board fee, meaning that hospitals charge the same fee regardless of how many nurses are employed in the patient’s care. In this model, nurses end up on the other side of hospitals’ balance sheets: a labor expense rather than a source of income.
For beleaguered administrators looking to sustain quality of care while minimizing costs (and maximizing profits), hiring and retaining nursing staff has arguably become something of a zero-sum game in the U.S.
But might the balance sheet in fact be skewed in some way? Could there be potential financial losses attached to nurse understaffing that administrators should factor into their hiring and remuneration decisions?
Research by Goizueta Professors Diwas KC and Donald Lee, as well as recent Goizueta PhD graduates Hao Ding 24PhD (Auburn University) and Sokol Tushe 23PhD (Muma College of Business), would suggest there are. Their new peer-reviewed publication* finds that increasing a single nurse’s workload by just one patient creates a 17% service slowdown for all other patients under that nurse’s care. Looking at the data another way, having one additional nurse on duty during the busiest shift (typically between 7am and 7pm) speeds up emergency department work and frees up capacity to treat more patients such that hospitals could be looking at a major increase in revenue. The researchers calculate that this productivity gain could equate to a net increase of $470,000 per 10,000 patient visits—and savings to the tune of $160,000 in lost earnings for the same number of patients as wait times are reduced.
“A lot of the debate around nursing in the U.S. has focused on the loss of quality in care, which is hugely important,” says Diwas KC.
But looking at the crisis through a productivity lens means we’re also able to understand the very real economic value that nurses bring too: the revenue increases that come with capacity gains.Diwas KC, Goizueta Foundation Term Professor of Information Systems & Operations Management
“Our findings challenge the predominant thinking around nursing as a cost,” adds Lee. “What we see is that investing in nursing staff more than pays for itself in downstream financial benefits for hospitals. It is effectively a win-win-win for patients, nurses, and healthcare providers.”
To get to these findings, the researchers analyzed a high-resolution dataset on patient flow through a large U.S. teaching hospital. They looked at the real-time workloads of physicians and nurses working in the emergency department between April 2018 and March 2019, factoring in variables such as patient demographics and severity of complaint or illness. Tracking patients from admission to triage and on to treatment, the researchers were able to tease out the impact that the number of nurses and physicians on duty had on patient throughput. Using a novel machine learning technique developed at Goizueta by Lee, they were able to identify the effect of increasing or reducing the workforce. The contrast between physicians and nursing staff is stark, says Tushe.
“When you have fewer nurses on duty, capacity and patient throughput drops by an order of magnitude—far, far more than when reducing the number of doctors. Our results show that for every additional patient the nurse is responsible for, service speed falls by 17%. That compares to just 1.4% if you add one patient to the workload of an attending physician. In other words, nurses’ impact on productivity in the emergency department is more than eight times greater.”
Adding an additional nurse to the workforce, on the other hand, increases capacity appreciably. And as more patients are treated faster, hospitals can expect a concomitant uptick in revenue, says KC.
“It’s well documented that cutting down wait time equates to more patients treated and more income. Previous research shows that reducing service time by 15 minutes per 30,000 patient visits translates to $1.4 million in extra revenue for a hospital.”
In our study, we calculate that staffing one additional nurse in the 7am to 7pm emergency department shift reduces wait time by 23 minutes, so hospitals could be looking at an increase of $2.33 million per year.Diwas KC
This far eclipses the costs associated with hiring one additional nurse, says Lee.
“According to 2022 U.S. Bureau of Labor Statistics, the average nursing salary in the U.S. is $83,000. Fringe benefits account for an additional 50% of the base salary. The total cost of adding one nurse during the 7am to 7pm shift is $310,000 (for 2.5 full-time employees). When you do the math, it is clear. The net hospital gain is $2 million for the hospital in our study. Or $470,000 per 10,000 patient visits.”
These findings should provide compelling food for thought both to healthcare administrators and U.S. policymakers. For too long, the latter have fixated on the upstream costs, without exploring the downstream benefits of nursing services, say the researchers. Their study, the first to quantify the economic value of nurses in the U.S., asks “better questions,” argues Tushe; exploiting newly available data and analytics to reveal incontrovertible financial benefits that attach to hiring—and compensating—more nurses in American hospitals.
We know that a lot of nurses are leaving the profession not just because of cuts and burnout, but also because of lower pay. We would say to administrators struggling to hire talented nurses to review current wage offers, because our analysis suggests that the economic surplus from hiring more nurses could be readily applied to retention pay rises also.Sokol Tushe 23PhD, Muma College of Business
For state-level decision makers, Lee has additional words of advice.
“In 2004, California mandated minimum nurse-to-patient ratios in hospitals. Since then, six more states have added some form of minimum ratio requirement. The evidence is that this has been beneficial to patient outcomes and nurse job satisfaction. Our research now adds an economic dimension to the list of benefits as well. Ipso facto, policymakers ought to consider wider adoption of minimum nurse-to-patient ratios.”
However, decision makers go about tackling the shortage of nurses in the U.S., they should go about it fast and soon, says KC.
“This is a healthcare crisis that is only set to become more acute in the near future. As our demographics shift and our population starts again out, demand for quality will increase. So too must the supply of care capacity. But what we are seeing is the nursing staffing situation in the U.S. moving in the opposite direction. All of this is manifesting in the emergency department. That’s where wait times are getting longer, mistakes are being made, and overworked nurses are quitting. It is creating a vicious cycle that needs to be broken.”
Goizueta faculty apply their expertise and knowledge to solving problems that society—and the world—face. Learn more about faculty research at Goizueta.
*Ding, Tushe, Kc, Lee: “Frontiers in Operations: Valuing nursing productivity in emergency departments.” Manufacturing & Service Operations Management 26:4:1323-1337 (2024)

Georgia could see the largest shortage of RNs by 2036
Staffing is one of the biggest issues facing ASCs. A 2023 survey from ORManager found that in the last 12 months, 56% of ASCs reported an increase in volume. Despite this success, 68% of facilities also reported having a more difficult time recruiting experienced operating room nurses.
“I think the biggest threat towards ASCs in 2023 is staffing, especially qualified, experienced staffing in all areas of an ASC, including business office, pre-op, OR (both nursing and surgical technicians), post-anesthesia care unit and recovery nurses. In addition, sterile processing technicians,” Michael Powers, administrator of Knoxville, Tenn.-based Children’s West Surgery Center, told Becker’s. “Each of these areas require a certain set of skills that are acquired and honed over time. There is increased competition, and in fact it is hard to compete with large health systems/hospitals. I am also finding that ASCs are competing in the same region against one another for the available staffing pool.”
The HRSA report highlights nurse workforce projections from 2021 to 2036 generated using the agency’s health workforce simulation.
Here are the five states with the largest projected shortages of registered nurses by 2036, per the report:
1. Georgia: 29% projected shortage
Projected vacancies: 34,800
2. California: 26% projected shortage
Projected vacancies: 106,310
3. Washington: 26% projected shortage
Projected vacancies: 22,700
4. New Jersey: 25% projected shortage
Projected vacancies: 24,450
5. North Carolina: 23% projected shortage
Projected vacancies: 31,350
https://www.beckersasc.com/leadership/5-states-facing-the-biggest-nurse-shortages-by-2036

Nursing Shortage Fact Sheet
The U.S. is projected to experience a shortage of Registered Nurses (RNs) that is expected to intensify as Baby Boomers age and the need for health care grows. Compounding the problem is the fact that nursing schools across the country are struggling to expand capacity to meet the rising demand for care. The American Association of Colleges of Nursing (AACN) is working with schools, policy makers, nursing organizations, and the media to bring attention to this healthcare concern. AACN is leveraging its resources to shape legislation, identify strategies, and form collaborations to address the shortage.
For more information including below, see attached PDF:
- Current and Projected Shortage Indicators
- Contributing Factors Impacting the Nursing Shortage
- Impact of Nurse Staffing on Patient Care
- Efforts to Address the Nursing Shortage
The cost of nurse turnover in 24 numbers
The 2024 NSI National Health Care Retention & RN Staffing Report features input from 400 hospitals in 36 states on registered nurse turnover, retention, vacancy rates, recruitment metrics and staffing strategies.
It found the average cost of turnover for one staff RN grew from January through December 2023 to $56,300, among other dollar figures and statistics that are helpful to understand the financial implications of one of healthcare’s most challenging labor disruptions.
Here are 24 numbers that illustrate the cost of nurse turnover, according to the most recent edition of the report, which is available in full here.
1. The turnover rate for staff RNs decreased by 4.6% in 2023, resulting in a national average of 18.4%. Given varying bed size, RN turnover can range from 5.6% to 38.8%.
2. The average cost of turnover for a staff RN increased by 7.5% in the past year to $56,300, with a range of $45,100 to $67,500. This is up from the average cost of turnover for an RN in 2022, which was $52,350.
3. Each percent change in RN turnover stands to cost or save the average hospital $262,500 per year.
4. The RN vacancy rate sits at 9.9% nationally. This marks an improvement, as hospitals hired an additional 153,000 RNs in 2023 and lowered the vacancy rate by 5.8%.
5. The average time to recruit an experienced RN ranges from 59 to 109 days, with the average for 2023 sitting at 86 days — nine days quicker than the year prior.
7. Every region represented in the 2024 report recorded a decrease to RN turnover, ranging from -1% to -5.1%. The South Central region saw the high end of this range while the North Central region saw the low end.
8. Over the past five years, RNs in step down, emergency services, and telemetry were most mobile with a cumulative turnover rate between 112% and 119%. “Essentially, these departments will turn over their entire RN staff in less than four and a half years,” the report states.
9. RNs in pediatrics, surgical services, and women’s health were less mobile, with 2023 turnover rates of 13.3%, 15.4% and 16.3%, respectively.
https://www.beckershospitalreview.com/finance/the-cost-of-nurse-turnover-in-24-numbers-2024
Costs and cost-effectiveness of improved nurse staffing levels and skill mix in acute hospitals
Extensive research shows associations between increased nurse staffing levels, skill mix and patient outcomes. However, showing that improved staffing levels are linked to improved outcomes is not sufficient to provide a case for increasing them. This review of economic studies in acute hospitals aims to identify costs and consequences associated with different nurse staffing configurations in hospitals.
Although more evidence on cost-effectiveness is still needed, increases in absolute or relative numbers of registered nurses in general medical and surgical wards have the potential to be highly cost-effective. The preponderance of the evidence suggests that increasing the proportion of registered nurses is associated with improved outcomes and, potentially, reduced net cost. Conversely, policies that lead to a reduction in the proportion of registered nurses in nursing teams could give worse outcomes at increased costs and there is no evidence that such approaches are cost-effective. In an era of registered nurse scarcity, these results favour investment in registered nurse supply as opposed to using lesser qualified staff as substitutes, especially where baseline nurse staffing and skill mix are low.
https://www.sciencedirect.com/science/article/pii/S0020748923001669
American Hospital Association Health Care Workforce Scan
The pandemic exacerbated existing shortages of health care workers in all roles, from clinicians to environmental and food services to admissions and scheduling. These shortages will persist well beyond the pandemic given today’s highly competitive labor market.
Record numbers of people are leaving their current jobs for new ones, new fields or new pursuits outside the job market altogether.
Despite all the difficulties, trauma and challenges they have faced, millions continue to show up and believe in their ability to make a difference in patients’ lives. Their mental and physical well-being requires tangible help and support from their leaders, and respect from the communities they serve.
The incredible challenges have also created unique opportunities to accelerate change and improve the way care is delivered, whether through technology, new care delivery approaches or multidisciplinary team models.
Ensuring the health and safety of the health care workforce – and the health and safety of the patients they care for – requires commitment at the individual, organizational and community level.

The Real Costs of Healthcare Staff Turnover
Staffing tops the list of healthcare industry challenges heading into 2023, according to polling data from healthcare advocacy group MGMA. It’s no wonder: Hospital staff turnover rates climbed as high as 26% in 2021 as workers retired due to burnout or went to work for organizations offering higher pay or better work-life balance.
For healthcare organizations, high employee turnover rates are a burden on finances and resources. Turnover costs include the expense of recruiting, hiring, and training new employees, as well as the cost of temporarily filling staffing gaps with expensive contract workers. There’s also the cost of reduced productivity as managers shift much of their attention to hiring and as new hires get up to speed. A less tangible—but still significant—turnover cost is lower employee morale as those who remain work harder to fill gaps for less pay than contract workers hired to provide temporary coverage.
Employee turnover refers to the total number of workers who leave a company over a specific period of time. Companies measure involuntary departures (layoffs and firings) and voluntary turnover (resignations) as well as the cost of replacing a given type of employee. Considering turnover can provide opportunities to replace underperformers, many employers also calculate the ideal turnover rate for their organization so managers can set specific employee retention goals. Every company has employee turnover—farsighted companies take the time to understand their turnover rate, the factors driving turnover, and what they can do to build and retain a workforce that will help achieve their organizational goals.
Key Takeaways
- Even before COVID-19, more than half of doctors and nurses reported symptoms of burnout, defined by physical and/or emotional exhaustion due to the rigors of the profession. But the pandemic shifted burnout into overdrive. During the pandemic, 93% of health workers reported experiencing stress.
- The average cost of turnover for a regular position is between six and nine months of an employee’s salary. Replacing a highly specialized healthcare professional can cost as much as 200% of the employee’s yearly salary.
- Patients notice high turnover rates when they see the impact of poor patient-to-staff ratios. They lose confidence in their healthcare provider when they don’t believe they’re receiving the best care, which can cause reputational damage.
In 2022, turnover rates for segments of the healthcare industry ranged from 19.5% at hospitals to 65% for at-home care providers to 94% at nursing homes.
This level of turnover puts a huge financial and logistical burden on healthcare providers. While COVID-19 put additional stress on the healthcare labor force, and the industry will likely feel the effects of COVID for years to come, the healthcare staffing crisis existed long before the pandemic. The following factors are also contributing to today’s healthcare worker exodus:
Inflexible, demanding schedules
Healthcare jobs are notorious for long hours and erratic schedules, and many are considered “deskless” jobs, meaning workers spend much of their time on the move. In fact, it’s estimated that nurses in hospitals walk about five miles a day.
Excessive administrative work
Fictional doctors and nurses are often depicted standing by a patient’s bedside, developing personal relationships and providing hands-on care. In reality, providers no longer have sufficient time to spend one-on-one with patients and other caregivers. Instead, they’re burdened by documentation, charting, and other administrative tasks. In 2021 doctors reported spending, on average, 15.6 hours per week on paperwork and other administrative tasks. First-year medical residents spend only about 10% of their work time face-to-face with patients, according to a study from Penn Medicine and Johns Hopkins University.
Heavy workloads
Even before COVID-19, more than half of nurses and physicians reported symptoms of burnout, according to the U.S. Department of Health and Human Services, and burnout rates have worsened over the past several years due to heavy workloads and related job stress. (A person experiencing burnout suffers from emotional exhaustion, depersonalization—a sense of detachment from oneself—and a reduced sense of personal accomplishment.) During the pandemic, researchers found that 93% of health workers were experiencing stress, 86% had anxiety, and 76% reported exhaustion.
Disconnection from managers
Healthcare workers who don’t work in a single location, such as nurses, medical assistants, and respiratory therapists, may miss out on opportunities to interact with their managers in person. Cut off from these critical personal connections, they can feel underappreciated and unseen, which makes it more likely they’ll look for a job elsewhere.
Relatively low pay
Many nurses feel they aren’t getting the pay they deserve. Even with a median annual salary of US$77,600, 66% of nurses describe pay as their No. 1 consideration when planning their next career move, according to a survey by Vivian, a healthcare hiring platform.
The direct costs of high employee turnover—the costs of recruiting, onboarding, and training new people and the costs of hiring contract staff to fill empty positions—are relatively easy to measure. The indirect costs are less quantifiable but just as burdensome; they include reduced patient satisfaction and lower employee morale. Consider these costs as you assess the impact of employee turnover on your organization.
1. Separation costs
These include severance pay, costs associated with unemployment insurance claims, payments for any ongoing benefits, and the costs associated with exit interviews and removing employees from all internal systems and directories.
2. Hiring costs
Turnover costs an organization much more than money. There’s the cost of reduced productivity when an employee leaves, and the hiring process itself can be expensive and resource intensive. It costs an employer an average of between six and nine months of an employee’s annual salary to replace them, according to the Society for Human Resource Management, and it can cost as much as 200% of the employee’s annual pay to replace a specialized healthcare professional.
3. Training costs
Even highly skilled and experienced employees need time to adapt to a new job. The healthcare industry has mandatory training and certification requirements that don’t exist in other industries. Unfortunately, many healthcare employees don’t feel they’re getting the right skills training for their rapidly changing roles, and managers and healthcare HR teams struggle to track and enforce training requirements.
4. Contingent labor costs
Understaffed healthcare organizations often resort to hiring travel or contract staff to fill workforce gaps. Unfamiliar with a facility’s policies, staff, and even its geography, contract workers can reduce overall productivity and burden full-time employees.
5. Substandard patient care
High employee turnover can lead to unsafe staff-to-patient ratios that make it hard to provide the best care. With too many patients to monitor, nurses and aides can overlook issues that slow recovery times and endanger patients. A study by the US National Institutes of Health showed that patients can lose confidence in their healthcare provider when they don’t believe they’re receiving the best care, which can tarnish the provider’s reputation.
6. Lower morale
The US healthcare industry lost more than 500,000 employees each month in 2022, according to the U.S. Bureau of Labor Statistics, and those left behind are dispirited about the future. In 2021, nearly three quarters of healthcare employees surveyed by Vivian, a healthcare hiring platform, said that workplace morale had gotten worse over the previous 12 months, and only 20% said they’re optimistic about the future of healthcare in the US. This lack of employee engagement is likely to increase employee turnover rates and reduce patient care levels, negatively impacting a healthcare organization’s reputation and financial health.
To reduce healthcare staff turnover (PDF), organizations must first improve employee well-being. People want to be compensated fairly, but beyond that, they want to be surrounded by coworkers and managers they respect. They want to feel ownership of their work lives and find work-life balance. They want systems and processes that are easy to navigate so they can focus on what matters—patient care. Here are some steps healthcare organizations can take to reduce turnover.
Managers who practice intentional hiring take the time to develop a clear job description for an open role and a clear plan for finding the right set of candidates. It may feel like this preparation lengthens the hiring process, but in the long run, it will pay off for the organization and for the candidates’ coworkers.
There are complications inherent in managing any 24/7 workforce, but these complications are compounded in healthcare by the need to have people with specific education, training, and certifications present at all times. The latest cloud-based human capital management (HCM) systems give managers visibility into staffing needs and availability and allow them to anticipate and cover surges.
Giving new employees the right tools at the start allows them to get a clear sense of the organization’s training goals and how they can fit training requirements into their workday. Dashboards that show employees what training they need, and when they need it, can improve compliance numbers while showing HR staff who’s falling behind. Cloud-based HCM systems let employees set their own training pace and measure their progress, which is especially valuable in busy workplaces where staff may have limited time to devote to training.
Healthcare professionals look for organizations that offer professional development programs beyond what’s required by law, including courses in management, communications, and ethics.
The stress of logging long hours in challenging situations is compounded by having to use inflexible, out-of-date, unconnected systems. Prospect Medical Holdings, which operates 17 hospitals and 165 medical care clinics across five states, at one time had 37 different HCM systems before successfully centralizing operations on a single cloud platform. A cloud HCM system enables employees to choose flexible schedules, sends workers notifications when it’s time to take a break, and allows management to send out regular communications that make workers feel more connected to the organization.
Healthcare-specific recruiting features in Oracle Fusion Cloud HCM help hospitals and other providers attract the best doctors, nurses, physician assistants, therapists, technicians, and support staff while giving them the tools they need to retain their accreditations and grow their expertise.
Oracle Cloud HCM’s workforce management capability enables staff to manage their schedules, sign up for shifts on their mobile devices, and block off time when they’re not available—giving them the ability to manage when and where they work. Healthcare providers can also use the cloud application’s dashboards to stay informed about patient counts and resource requirements so they can make shift changes as needed. Additionally, Oracle Cloud HCM’s employee experience platform makes it easy for hospital leaders to keep employees informed about significant organizational news and initiatives and, through pulse surveys, learn about employee concerns and needs.
Technology alone will never solve the healthcare industry’s employee turnover problem. That will take concerted efforts by healthcare organizations to focus on staff well-being, open up lines of communication, and improve the workday experience. But the right technology—easy to use, mobile friendly, and able to take on the most monotonous administrative tasks—can make a huge difference, allowing staff to focus on more complex and rewarding work: caring for patients.
Learn how the Oracle ME platform can help your organization improve the employee experience.
What is the cost of employee turnover generally?
Employee turnover costs US companies an average of $50,000 per worker, not factoring in the heavy burden on the employees who stay.
How is the cost of employee turnover calculated?
To calculate turnover costs, dig into the numbers. Calculate the cost to hire contract fill-ins for the vacant position and the cost to recruit and hire the new employee (including job postings, managerial and HR time, and background screenings). Also factor in onboarding and training costs, as well as productivity costs as the new hire ramps up. The latter is usually calculated as the cost of a new hire’s salary and benefits during their first 30 to 90 days, when they’re doing more training than work.
What is the cost of nurse turnover?
The average cost of turnover for a staff registered nurse in the US is $46,100, with an average range of $33,900 to $58,300, according to the 2022 NSI National Health Care Retention and RN Staffing Report from Nursing Solutions Inc., a national nurse recruitment agency. The average time needed to replace a nurse is about 87 days. Nurses in some fields, including emergency services and behavioral health, are leaving at accelerating rates, with cumulative turnover rates that exceed 100%. (This happens when jobs need to be filled over and over—for example, an organization with 100 employees may have 50 positions that are filled by employees who stay long term and 50 positions where lots of turnover is the norm. Each terminated employee is part of the organization’s overall turnover rate.)
https://www.oracle.com/human-capital-management/cost-employee-turnover-healthcare

The Relationship Between Nurse Staffing, Quality, And Financial Performance In Hospitals
Little evidence exists on the relationship of nurse staffing and quality with financial performance in hospitals. This study aimed to measure the relationship between nurse staffing, quality of care, and
profitability in hospitals. This study used longitudinal panel datasets from 2006 to 2010, drawn from various datasets including the American Hospital Association Annual Survey Database, Medicare Cost Report, and Hospital Compare Data. This study used the random-effects linear regression model to measure the relationship between nurse staffing, quality, and profitability. In addition, we tested a mediating effect of quality on the relationship between nurse staffing and profitability. This study found nurse staffing’s significant association with quality and profitability in hospitals. First, compared to hospitals in the lowest quintile of RNs per 1,000 inpatient days, hospitals in the higher quintiles had lower pneumonia readmission rates, and higher total profit margins, operating margins, and cash flow margins. In addition, hospitals with lower pneumonia readmission rates were found to have higher total profit margins and cash flow margins. Lastly, the current study found that the positive relationship between RNs per 1,000 inpatient days and total profit margin and cash flow margin was partially mediated by pneumonia readmission rates. In conclusion, our finding that nurse staffing is positively associated with both quality of care and profitability in hospitals suggests that the idea of hospitals responding to financial pressures by cutting RN resources with a goal of greater profitability should be called into question. The influence of lower RN staffing levels on higher profitability for hospitals is uncertain, while it is possible that RN staff reductions may compromise the quality of patient care. Keywords: nurse staffing, registered nurse, quality of care, readmission rate, profitability, total profit margin, operating margin, cash flow margin, hospital.
On a practical level, the findings on the relationship between nurse staffing, and the quality and financial outcomes in hospitals can assist nurse managers and chief executive officers in identifying the optimal RN staffing level. These findings suggest that RN staffing level may be a strong predictor of quality and profitability and that the quality may mediate the relationship between RN staffing level and profitability in hospitals. This could be of particular interest to current hospital managers because of the payment reductions for excessive readmissions embedded in the ACA, which might have significantly affected the average profitability of some service lines in their hospitals. A lesson that can be learned from the past is that hospitals may attempt staff reductions in response to increased financial pressures as a result of payment reforms. However, as the findings in this research and the literature suggest, the reduction of nursing staffs may be related to an increase in adverse effect on the quality of patient care. The analysis results of this study demonstrated that a higher RN staffing level was associated with a lower pneumonia readmission rate, while the medium level of RN staffing level (≈ 7.7 RNs per inpatient day) had the highest profitability among general and acute care, non-federal government hospitals. Staffing decisions involve balancing between labor costs and the level of care required to fulfill healthcare needs of patients (Blegen, Vaughn, & Vojir, 2008). It is a matter of choice to hospital managers to decide what would be the most effective nurse staffing strategy for their hospitals in response to the HRRP.
https://journals.scholarpublishing.org/index.php/ABR/article/view/8745

The Effects of Nurse Staffing on Hospital Financial Performance: Competitive Versus Less Competitive Markets
Hospitals facing financial uncertainty have sought to reduce nurse staffing as a way to increase profitability. However, nurse staffing has been found to be important in terms of quality of patient care and nursing related outcomes. Nurse staffing can provide a competitive advantage to hospitals and as a result better financial performance, particularly in more competitive markets
In this study we build on the Resource-Based View of the Firm to determine the effect of nurse staffing on total profit margin in more competitive and less competitive hospital markets in Florida.
By combining a Florida statewide nursing survey with the American Hospital Association Annual Survey and the Area Resource File, three separate multivariate linear regression models were conducted to determine the effect of nurse staffing on financial performance while accounting for market competitiveness. The analysis was limited to acute care hospitals.
Nurse staffing levels had a positive association with financial performance (β=3.3; p=0.02) in competitive hospital markets, but no significant association was found in less competitive hospital markets.

Optimizing the Role of Nursing Staff to Enhance Physician Productivity: One Physician’s Journey
After completing my family medicine residency a few years ago, I immediately joined a private group practice with eight family physicians and two nurse practitioners and inherited a nearly full patient panel from a retiring family physician. I naively assumed that transitioning from residency to private practice would decrease my workload and increase my quality of life, but after a hectic first year, I knew that something had to change for my professional life to be sustainable. I was spending way too much time working and could see that the complexity of practicing medicine would continue to increase in the years ahead.
I began to look for ways to cope and came across an article in Family Practice Management by Peter Anderson, MD, and Marc D. Halley, MBA.1 The article described a new model in which a physician works simultaneously with two clinical assistants – a registered nurse (RN), a licensed practical nurse (LPN), or even a capable medical assistant (MA) – allowing them to assume more responsibility for each patient encounter so the physician can focus on the patient and medical decision-making. The additional nurse responsibilities include gathering an initial history (including the history of present illness, HPI; review of systems; past medical, social, and family history, PSFH; and health habits) and then staying in the exam room to document the physician encounter, order needed tests, print handouts, send prescriptions to the pharmacy, and complete the note including the assessment and plan. By shifting many of the ancillary physician tasks to well-trained clinical assistants, the physician can focus on what he or she is uniquely trained to do – provide high-quality acute, chronic, and preventive care in the context of a therapeutic relationship. After discussing this idea with my nurse (an LPN) and practice manager, we decided to try this new model.
My nurse and I started slowly, selecting several days where we would see fewer patients, thereby allowing additional time to learn our new process. It was a significant adjustment for both of us. She was now in charge of the documentation (and thus the computer), and it became necessary for me to clearly verbalize every aspect of the visit, including the physical exam, the assessment, and the plan for treatment or additional workup (labs, imaging, medications, referrals, etc.). We used Anderson and Halley’s model as our starting point, but soon our process evolved based on our own skills and strengths, the needs of our patients, and the limitations of our office space, schedule, and electronic health record (EHR). After experimenting for a month, we were both convinced that we were ready to fully commit to this new model and decided to hire a second nurse. Because we had spent significant time fine-tuning our system, the training process for our second nurse (also an LPN) was relatively smooth, and my original nurse was able to do the bulk of the teaching.
Every new process requires some experimentation and modification in the early stages, and for our practice key adjustments occurred in the following areas:
Communication with nurses. When we first began, I would handwrite my assessment and plan for each patient encounter to ensure accuracy. Quickly, my nurses let me know that this was a waste of time. Instead, they suggested that I clearly explain each diagnosis and associated plan to the patient, and they would capture the information as I spoke. The nurses have also demonstrated that they can capture patient instructions as we discuss them, and they now typically print those instructions at the conclusion of each visit. Today it is unusual for me to type or handwrite anything during an office visit.
Access to patient data. Each of our exam rooms has a desktop computer that we use to navigate the EHR. Lab and imaging results import electronically into the EHR, as do many of our consult notes. With my nurse in the room using the computer during the office visit, I lost the ability to peruse the chart during the visit, so I began to use an iPad with our wireless Internet connection to view a read-only version of the chart. The iPad also allows me to review the history related to each problem, the problem list, and current medications without pulling my nurse away from her documentation responsibilities.
Chart review. As we progressed with our new model, I continued to gradually shift more responsibility onto my nurses’ capable shoulders. They assumed responsibility for immunization status (checking status for adults and children, administering needed vaccines, creating catchup schedules, etc.), preventive care, and even some basic chronic disease management (confirming annual diabetic eye exams and referring as needed, ordering annual lipid panels when appropriate, etc.). The nurses found that in opening a visit note, they were essentially doing a thorough chart review including reviewing, updating, and sorting the problem list; reviewing preventive care needs; sorting the medication list; reviewing and reorganizing the PFSH and health habits; starting the HPI by searching the chart for any prior tests or visits related to the chief complaint (as recorded by the front desk staff when scheduling the visit); and even starting the assessment and plan portion of the note by listing the relevant diagnoses. It was not possible to accurately complete such a chart review between patients, so my nurses agreed to arrive about an hour before our first patient each day to allow additional time for this work.
Patient check-in form. We have continually worked to implement processes that improve patient flow and efficiency during office visits. One of our more successful processes involves using a patient check-in form. Early on, it became apparent that the rooming process was a bottleneck in our patient flow because of the need to confirm problems, medications, allergies, social history, family history, habits, etc. I had asked my nurses to attempt to quickly update these at each office visit, and it turned into a time-consuming process, particularly for complex patients on multiple medications. To expedite the process, we worked with our EHR support staff to create a one-page document that lists a patient’s medications, allergies, family history, social history, health habits/risk factors, pharmacy of choice, and advance directives. These forms are printed directly from the EHR during the morning chart review and are given to the front desk staff to pass out to patients when they arrive. This allows patients to review much of their history while sitting in the waiting room and allows the nurses to address only changes that need to be made. As an added benefit, patients appreciate that we put time into prepping for their arrival rather than handing them a blank form to complete.
Patient privacy. I was concerned that having a nurse present in the exam room might be a distraction for patients or make them uncomfortable sharing sensitive information. While we did receive several questions initially about the nurse being in the room, I have been pleasantly surprised by how many patients don’t even seem to notice. There are occasional instances when it is evident that a patient would be more comfortable without a nurse present during the visit, and the nurses can usually ascertain this while rooming the patient. Overall, feedback has been amazingly positive. Rather than viewing the nurses as an intrusion, patients appreciate the additional resources that my nurses have become. They also seem to recognize that the nurses’ presence allows me to be fully focused on them, rather than trying to manage charting, test orders, referrals, and refills while providing their care.
Space, workflow, and scheduling issues. Because my colleagues were not implementing the same practice model that I was, I was careful to limit the impact on them. To create a new workspace for my second nurse, I cleared some supplies from an unused desk, purchased a new computer, purchased a new office chair, and moved an unused phone. I typically have access to only two or three exam rooms while seeing patients (the Anderson and Halley model suggests three to five exam rooms), but I have not asked for more. I have found that even with two exam rooms I am considerably more efficient under this model.
While both of my nurses participate in patient visits throughout the day, they typically have short breaks between patients and can use this time to manage phone calls, medication refills, and other peripheral nursing issues. Because of this, we have not needed to schedule additional time for the nurses to manage these tasks, although we have utilized our group’s two full-time triage nurses for support on our most hectic days.
The transition to our new model has probably been most difficult for our office manager and our group’s lead nurse. A new process was required to schedule my nurses, and it can be tedious to manage schedules when I am out or one of my nurses is out. I have just recently started training some of our other office nurses in the new model, but previously I would have to resort to my old single-nurse system if one of my two nurses was out of the office.
Ongoing improvement. To fully implement this system requires nurses who are motivated and willing to assume more ownership over each patient encounter. The nurses’ knowledge of each patient and their overall medical knowledge has grown as a result of their active participation in each visit, and they have learned by watching how I make decisions and conduct the medical workup. I also continue to teach them in a more formal manner by using interesting cases that we see, and I have learned this model requires an ongoing commitment to training. I started out meeting with my nurses for one hour each week, and even though I have been using this system for almost two years, I continue to meet with them at least twice per month. During these meetings I elicit feedback about problems or inefficiencies, provide feedback on recent chart notes, and provide teaching about changing medical standards of care. My nurses are now often the ones to identify problems and suggest appropriate changes to improve our model and the care we provide. These routine meetings have created a culture of teamwork and a continual focus on innovation – traits that will likely serve us well in the ever-changing world of medicine.
Two years into the model, we can report positive results.
Patient care statistics. The organization I work for monitors patient care data, generating physician report cards for preventive care and chronic disease management. Since implementing this new practice model, I have seen an improvement in most of my report card measures, particularly those that rely more on my nurses to complete. For example, the table below shows improvements in virtually every category of diabetes care, with a particularly large jump in the percentage of diabetes patients who have received foot exams, a task I have completely turned over to my nurses.
Since implementing my new practice model, in which nurses take greater responsibility for certain aspects of the patient visit, I have seen improvements in most of my report card measures, including those for diabetes care, shown here.
| Percentage of diabetes patients | |||
|---|---|---|---|
| Diabetes measures | Goal | Old system | New system |
| A1C > 9% | < 15% | 5% | 0% |
| A1C < 7% | > 40% | 53% | 64% |
| Blood pressure > 140/90 mm Hg | < 35% | 22% | 7% |
| Blood pressure < 130/80 mm Hg | > 25% | 53% | 64% |
| Eye examination completed | > 60% | 47% | 48% |
| Smoking status and cessation advice or treatment provided | > 80% | 98% | 98% |
| LDL > than 130 mg/dl | < 37% | 15% | 9% |
| LDL < 100 mg/dl | > 36% | 58% | 62% |
| Nephropathy assessment completed | > 80% | 95% | 95% |
| Foot examination completed | > 80% | 60% | 79% |
Finances and productivity. The costs incurred with this new model can be divided into two categories: initial startup costs and ongoing costs. I estimate that my initial startup costs were in the range of $15,000. This includes the fairly nominal cost of additional office equipment (computer, office chair, etc.) and the more significant cost of slowing down my days as I brought both nurses up to speed on the new system. The only significant ongoing cost is paying the salary and benefits of my second LPN, approximately $8,000 per quarter. This is less than you might expect because four months after transitioning to this new model, I made a personal decision to decrease my full-time equivalent (FTE) status from 1.0 to 0.75. Thus, I am not responsible for the full salary of my second nurse. The remainder of her time is allocated to other parts of the practice.
My FTE change makes it nearly impossible to calculate how my practice change has affected revenue, but I can say that my office productivity has increased. We measure productivity in terms of patient visits per half-day and average charge per patient visit, which we track based on work relative value units (RVUs). Since moving to this new system, I have seen my patient visits per half-day increase by 15 percent and my average charge (work RVU) per office visit increase by 10 percent (see the graph below). Because some of our practice costs are divided based on productivity, this increase in my productivity has led to a relatively minor, but ongoing, increase in those costs.
Under my new practice model, patient visits per half-day have increased 15 percent and work relative value units (RVUs) have increased 10 percent. These numbers reflect an eight-month average before and after changing to the new model.
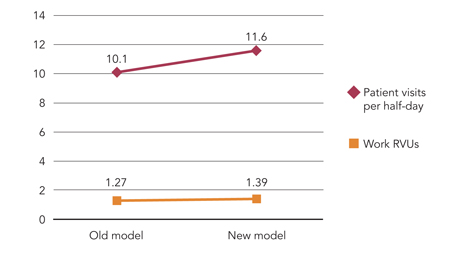
Although this new model has certainly brought an increase in expenses, I have seen a much greater increase in productivity and revenue, which has allowed me to maintain an annual income above the national median of $160,000 for a full-time family physician, despite having decreased my FTE status to 0.75.
Nurse and patient satisfaction. During this transition I have regularly asked my nurses for feedback regarding their satisfaction with our change, and when there have been frustrations or difficulties, I have done my best to work creatively with them to correct those. At this point, I am happy to report that my nurses are both very pleased with our current system. My original nurse reports that “Overall, I am very happy with the two nurse system. My favorite thing about it would be that I get to see from start to finish the entire diagnostic and treatment process. It allows me to become educated on each patient’s history and treatment plan, which in turn allows me to provide appropriate care and to be a better advocate for that patient. While working so closely together, I’ve been able to gain an understanding of how Dr. Anderson practices, and I have become more confident in myself and my own skills. Our care as a team has become significantly more thorough, and we are able to focus now on providing comprehensive care to each individual.”
Although we have not conducted a formal patient survey, the feedback we have received from patients has been almost universally positive. Patients are happy to have my undivided attention while in the exam room, they appreciate getting so much done with each office visit, and they are grateful that my increased efficiency has allowed me to be more available for same-day appointments.
This journey in restructuring my practice model has led me to a place where I am able to focus more on my patients, provide higher quality care, be more productive, and have happier employees. As physicians, we should not view ourselves as beholden to old models of care. Instead, we ought to view ourselves as empowered to institute fundamental changes to our work. The practice of family medicine is likely to get more demanding in the years ahead, and it is our opportunity and responsibility to build innovative practices that meet these demands while enabling excellent patient care, employee satisfaction, and a sustainable and meaningful personal life.

10 Best Practices for Increasing Hospital Profitability
Industry experts say that hospitals wishing to increase their profitability can focus on two key areas — reducing costs and increasing reimbursement. Here are 10 best practices for increasing hospital profitability by reducing costs and increasing revenue and reimbursement.
Because labor is the largest single expense for hospitals, it is critical that hospitals are not over- or under- staffing their facilities.
Hospitals leaders can cosider the use of flexible staffing, such as part-time or hourly employees, and adjust staffing based on patient census data. Leaders should also monitor the efficiency of this staffing by continuously reviewing benchmarking data such as hours worked per case.
Amy Floria, CFO of Goshen (Ind.) Health System, says that her facility monitors patient volume on a daily basis and adjusts staffing accordingly. “We adjust our nursing staffing every eight hours after looking at our inpatient volume and expected discharges and admits,” she says.
Kevin Burchill, a director at Beacon Partners, a healthcare management consulting firm, agrees that staffing must be adjusted daily. “The easiest thing that a hospital can do to improve profitability is for the senior management team to assume responsibility for the day-to-day performance of an organization and look at the organization’s performance in real time,” he says. “You must shift to an emphasis on the day-to-day, not pay-period to pay-period or month-to-month.”
It is important that concerns regarding efficient staffing are communicated throughout the organization and that hospital leaders work in collaboration with physicians. Donna Worsham, COO of National Surgical Hospitals, suggests that hospital leaders share staffing efficiency benchmarking data with unit managers and provide feedback regarding the productivity of the unit.
Flexible staffing is especially useful for OR nursing staff. OR managers should review clock-in times versus surgery-start times and determine if their staff is consistently arriving before a surgery actually begins. If this is the case, mangers can utilize flexible staffing to allow nursing staff to arrive later so that when surgeries run over, no overtime expenses are incurred, says Ms. Worsham.
Other facilities are saving in staffing costs by reducing benefits for full-time staff. Goshen Health System, for example, deferred merit increases, reduced paid vacation time and suspended its retirement matching program in response to the current economy, according to Goshen’s CEO, Jim Dague. Goshen reduced employee dissatisfaction in response to these cuts by soliciting employee feedback on which benefits to reduce, thereby building organizational support for the changes. In addition, Goshen’s executives took a voluntary 20 percent cut in order to help sustain the system through the recession.
Joe Freudenberger, CEO of OakBend Regional Medical Center in Richmond, Texas, agrees that staff must buy in to any reductions in hours and shifts worked that will personally affect them in order for the hospital to remain successful. He says that hospital leaders must communicate the reasoning for these changes to the staff before making them. “If we call off staff, they see it as personally hurting their income when we need to help them understand that it is actually preserving their income by maintaining the financial viability of the hospital,” he says. “It may be obvious to us that we’re calling them off because we have a significant reduction in patient volume, but we need to communicate that to them for them to understand the financial realties we face.”
Although some staffing cuts may be necessary, hospitals should be careful not to take a blanket approach to layoffs or cuts in services. Hospital leaders must take a close look at their business before making cuts.
“Don’t make the same mistake everyone else does — don’t look at bottom line, determine that you need to cut $1 million, for example, and then cut 10 percent across the board. Doing so will trim some fat but will cut meat and bone in other areas,” says Mr. Burchill.
He suggests that hospitals assess each program individually and determine which ones are what are winners and losers. “You do not want to cut areas that you should be doing more of or that are already profitable,” says Mr. Burchill.
Hospital leaders can reduce supply costs by working with vendors to improve contracts and encouraging physicians to make fiscally responsible supply decisions.
“When it comes to supply costs, you must drive this expense or the vendor will drive it for you,” says Ms. Worsham.
Hospital leaders should not shy away from approaching vendors for discounts. Goshen’s IT director recently requested a discount on the health system’s contract for IT maintenance due to current economic conditions and successfully received a discount that saved the hospital 15 percent on this contract, according to Ms. Floria.
Hospitals can also reduce supply costs be reducing the number of vendors. Goshen, for example, is in the process of reducing the number of vendors in its surgical suite and aims to eventually scale the vendors down to 4-6 companies. “This action is expected to save us at least a million dollars in supply costs,” says Mr. Dague.
Another way in which hospitals may reduce supply costs is by requiring vendors to submit purchase orders for any equipment or implants that are not included in a negotiated, written agreement with the facility. “All of our vendors sign agreements that any purchase orders must be submitted at least 24 hours before a procedure and must be approved by the materials manager or the CEO, or it’s free,” says Ms. Worsham. “If you don’t require this, vendors will drop off the invoice for a pricey piece of equipment or implant after the procedure has already taken place and walk out the back door, which can greatly hurt your profitability.”
All hospitals can benefit from tightening up the efficiency of their operating rooms, but it is especially critical that less busy facilities ensure that their ORs are used as efficiently as possible.
“Hospitals need to review block time utilization,” says Ms. Worsham. “Physicians who are assigned more time than they are using are hurting your profitability.”
Ms. Worsham suggests that hospital OR managers work directly with physicians to make OR utilization more efficient.
“When physicians’ schedules create gaps in the OR schedule, it effects a hospital’s ability to staff effectively, which can create significant labor costs for the hospital,” says Ms. Worsham.
Hospitals should work to encourage physicians to become more concerned about the costs of supplies and other activities, such as unnecessary tests and inefficient coding processes that may drive up hospital costs.
“Hospitals today have a unique opportunity to leverage physicians’ interest in having hospitals help to stabilize their incomes with the hospitals’ needs to involve physicians in cutting costs and improving quality,” says Nathan Kaufman, managing director of Kaufman Strategic Advisors, a hospital consulting firm.
Hospitals can encourage the use of products from vendors that are cost-effective, but still high quality, especially in areas such as orthopedic implants, which can be considerably costly for hospitals. In addition, experts say the use of protocol-based care can reduce costs associated with unnecessary tests or treatments.
Mr. Freudenberger says that one of the biggest mistakes hospitals make is not engaging medical staff in profitability. “Physicians have a huge role in maintaining hospital profitability, but unless you give them a reason to be concerned with a hospital’s profitability, they will make choices in what and to whom they refer services that will not consider the implications to the hospital,” says Mr. Freudenberger. “Hospital leaders should work to help medical staff understand the connection of their referrals to the hospital’s viability so that their referral decisions reflect the value they place on the hospital.”
During tough economic times, some hospitals may benefit from outsourcing or partnering with other organizations for certain services, such as food and laundry services, and even, in some cases, clinical services.
“Some hospitals see these economic times as an opportunity to outsource unprofitable services,” says Mr. Burchill.
By outsourcing certain services to more efficient providers, hospitals can share the savings with the service provider. However, hospitals must be sure to select truly efficient providers.
“Outsourcing is clearly a smart thing to do if an organization can gain greater efficiency through finding a larger-scale operation; however the provider must be more efficient than the hospital,” says Kevin Haeberle, executive vice president, HR capital, for Integrated Healthcare Strategies.
Oftentimes, hospitals outsource services such as laundry, food and nutrition, information technology or human resources because they do not have the capital to invest in the equipment upgrades or training that is needed to increase the efficiency of their internal service. In these cases, the decision to outsource may not directly be related to profitability but instead the “lacking of funds for the investment required to make current services viable,” says Mr. Haeberle. However, this decision can improve profitability in the long-run by allowing hospitals to use funds for more profitable services.
Some hospitals have also begun to outsource clinical services such as emergency room staffing and anesthesiology in an attempt to become more efficient. Because these staffing groups employ a large number of specialty physicians, they may be able to provide more efficient services, especially in clinical areas that require around-the-clock coverage where the demand for services is high.
Mike Mikhail, MD, vice president of client services for Emergency Physicians Medical Group, says that hiring an emergency department management company can help to improve the profitability of hospitals whose demand for emergency services exceeds its emergency treatment capabilities. “An emergency management group can help make the emergency department more efficient by introducing management oversight and best practices, allowing more patients to be seen and keeping others from leaving to find another hospital,” he says. “Because a majority of hospital admits come from emergency walk-ins, driving more patients through an ER will create more admits, and therefore more profit for the hospital.”
An increasing number of hospitals are joint venturing with local physicians and surgery center management companies to offer outpatient services through the development of a surgery center.
According to Clete Walker, vice president of development for Surgical Care Affiliates, hospitals are beginning to focus on the need for a comprehensive outpatient strategy and recognizing the need to partner with doctors to effectively execute on this strategy. Mr. Walker reports that he has seen an increased interest from hospitals in joint venture arrangements for outpatient services.
“More and more hospitals are realizing that their core competency is providing inpatient care; their outpatient cases are more costly per case and take up more of the physician’s and patient’s time than they do at an ASC,” he says. “As a result, hospitals are competing with physicians for outpatient cases. Hospitals with joint-venture agreements, however, do not have to compete with the physicians.”
Hospitals can leverage their standing in the community to partner with local physicians to share the revenue generated by efficient outpatient cases.
“We are in lean times, and lean times call for us to rethink our strategies,” says Mr. Walker. “It’s better for physicians, hospitals and other groups to work together to provide an efficient delivery system for patient care than for the groups to compete.”
Identifying and attracting additional physicians to bring cases to your hospital is another way that hospital leaders can increase profits. Physician-owned hospitals can bring in additional physicians as partners, while other types of facilities can recruit new physicians who are willing to perform cases at their hospitals.
“New physicians will bring in more cases and grow your profits,” says Ms. Worsham.
Ms. Worsham suggests polling your medical staff for names of local physicians to target and inviting them into the facility. During the visit, Ms. Worsham recommends that hospitals work to “wow” the target physician. “We work tirelessly to promote the services we can offer them,” she says.
When a new physician begins performing cases at one of Ms. Worsham’s facilities, that physician is assigned a concierge. “We have strong internal programs in place for this first day. A concierge is assigned to each new physician who provides them with a tour facility and walks them through every aspect of their day,” says Ms. Worsham.
Hospitals may also be able to grow case volume and profits by adding new service lines. However, hospitals need to be careful to do their homework on the expected profitability and ROI for any new lines added, especially in a market where access to the funds required to invest in new service lines may be tight.
“You have to look at what the market needs are and where you’re going to get the referrals from,” says Ms. Worsham. “Meet with local physicians and interview them about their needs and the number of cases they see that could utilize a new service.”
Hospitals should also be sure to examine the competitive landscape for any new service line.
Ms. Worsham reports that her facilities have had great success from adding a hyperbaric service line because few competitor hospitals were offering this service.
Hospitals that use hospitalists to care for patients can benefit from the more efficient care and better documentation that specialized hospitalists can potentially provide.
“A protocol-based hospitalist program can increase efficiency and help to reduce the length of stay for patients, which can increase case volume without the need for additional beds,” says Mr. Kaufman.
Hospitals should consider employing these specialists as a means to improving care and enhancing their bottom lines, according to Mr. Kaufman.
Stephen Houff, MD, president and CEO of Hospitalists Management Group, says that hospitalist groups can provide effective care to patients and possibly increase reimbursement. “Hospitalists may be the most reliable and cost-effective means available for hospital leaders to transform medical delivery in their health system,” he says. “Through shared vision, an effective hospitalist team partners with hospital leadership to improve patient safety and access, streamline care, improve patient and family satisfaction, enhance reimbursement via improved clinical documentation and provide seamless transition to post-discharge care.”
One of the most important ways that hospitals can improve their profitability is by continually evaluating and renegotiating their managed care contracts.
“Hospitals must demand their fair share of premiums from third-party payors in order to subsidize the underpayment of Medicare and Medicaid,” says Mr. Kaufman. “Hospitals need to focus on reducing their cost structure as much as possible to approach breaking even with Medicare reimbursement rates, but that only goes so far.”
Mr. Kaufman recommends that hospitals only agree to contracts that reimburse at 130-140 percent of cost. “If a facility is not big enough or strong enough to get these rates, then they should look at merging with a larger facility,” says Mr. Kaufman.
Ms. Worsham suggests that hospitals perform a profitability analysis by payor and by procedure in order to determine where a facility is losing money and identify any trends. She also suggests that hospitals evaluate older contracts due to changes in severity-based DRGs and carve out the reimbursement of implants in order to ensure they are reimbursed appropriately for the costs associated with these.
Ms. Worsham also suggests that hospitals evaluate contracts on a quarterly basis, even if the contract is not near expiring. She suggests that hospital leaders examine the contracts with the following questions in mind:
• Is revenue where we thought it would be given reimbursement rates and volume of policy holders?
• Are we being paid as agreed upon in the contract?
• Are we being paid in a timely manner?
Contracts that are determined to be “high risk” should be renegotiated. Make sure your contracts contains a material harm clause, which will allow you to readdress terms of contracts that have become financially harmful to the facility, according to Ms. Worsham. Renegotiating contracts can be very valuable — one hospital Ms. Worsham advises will gain $500,000 this year due to renegotiations.
Hospitals that focus on enacting these best practices are likely to see improvements in their profitability; however, hospitals can also benefit by using today’s economic conditions as an opportunity to improve their overarching approach to business, creating a more sustainable organization in the future.
“When profits were high, hospitals had the luxury of being sloppy in some areas; now we must run a tighter ship,” says Ms. Floria. “This will benefit the industry in the long-run.”
Hospitals can also use this opportunity to find creative solutions to problems that plague their facilities.
Goshen Health System, for example, recently enacted a program in which the hospital pays the premium required to sustain Cobra benefits for recently laid-off patients seeking care. “We are willing to be creative with our patients,” says Ms. Floria. “We pay for benefits when certain patients cannot. The revenue we receive from caring for these patients recoups this cost and provides us with additional cash flows that likely would have been uncollected or written off to charity care or bad debt.”
This idea, which was enacted during lean times to improve profitability, will continue to benefit the hospital’s bottom line, even when profitable times return.
Contact Lindsey Dunn at lindsey@beckersasc.com.